Abstract
Restenosis after coronary angioplasty arises from fibrocellular intimal hyperplasia and possibly failure of the artery to enlarge adequately. Which mechanisms underlie this process is only partly understood. No drugs have been clinically effective in reducing the incidence of restenosis. Since recently, photodynamic therapy (PDT) is being investigated as a possible treatment for intimal hyperplasia. PDT involves the systemic administration of a light-excitable photosensitizer that is takers up rather preferentially by rapidly proliferating cells. During laser irradiation light energy is transferred from the photosensitizer to oxygen generating the highly reactive singlet oxygen. This potent oxidizer can cause severe cellular damage. After PDT of a balloon-injured artery from the rat and rabbit the media remained acellular for several weeks to months, and intimal hyperplasia did not occur. The endothelial lining regenerated by two weeks, but why smooth muscle cells did not repopulated the media is not known.
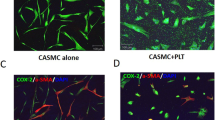
Neutrophils seem to play an important role in the prevention of restenosis after coronary angioplasty, since the activation status of this type of phagocyte is directly related to vessel diameter at late follow-up. Furthermore, it has been observed that neutrophils adhere to the microvascular wall upon PDT in vivo. In vitro findings suggest that the increased neutrophil adherence was not dependent on a decreased release of the anti-adhesive factors NO and prostacyclin by the PDT-treated endothelial cells. Furthermore, PDT did not stimulate the expression of P-selectin by the endothelial cells, one of the adhesion receptors for neutrophils. The endothelial cells only retract upon PDT allowing the adherence of neutrophils by their β2-integrin adhesion receptors to the subendothelial matrix. On the basis of these findings, we presume that the successful prevention of intimal hyperplasia by PDT partly depends on the presence of the neutrophil at the site of the lesion.
Similar content being viewed by others
References
Gruentzig AR, Myler RK, Hanna ES, Turina MI: Transluminal angioplasty of coronary-artery stenosis [Abstract]. Circulation 56 (suppl 11): 111–84, 1977
Lee PC, Gibbons GH, Dzau VJ: Cellular and molecular mechanisms of coronary artery disease. Coronary Artery Dis 4: 254–259, 1993
Forrester JS, Fishbein M, Helfant R, Fagin J: A paradigm for restenosis based on cell biology: clues for the development of new preventive therapies. J Am Coll Cardiol 17: 758–769, 1991
Serruys PW, Foley DP, Kirkeeide RL, King SB III: Restenosis revisited: insights provided by quantitative coronary angiography. Am Heart J 126: 1243–1267, 1993
Wong CS, Leon MB, Popma JJ: New device angioplasty: the impact on restenosis. Coronary Artery Dis 4: 243–253, 1993
Jackson CL: Animal models of restenosis. Trends Cardiovasc Med 4: 122–130, 1994
Clowes AW, Reidy MA: Prevention of stenosis after vascular reconstruction: pharmacologic control of intimal hyperplasia—A review. J Vasc Surg 13: 885–891, 1991
Popma JJ, Califf RM, Topol EJ: Clinical trials of restenosis after coronary angioplasty. Circulation 84: 1426–1436, 1991
Faxon DP, Currier JW: Prevention of post-PTCA restenosis. Ann NY Acad Sci 748: 419–427, 1995
Wanibuchi H, Dingemans KP, Becker AE, Ueda M, Naruko T, Tanizawa S, Nakamura K: Is the Watanabe Heritable Hyperlipidemic Rabbit a suitable experimental model for percutaneous transluminal coronary angioplasty in humans? A light microscopic, immunohistochemical and ultrastructural study. J Am Coll Cardiol 6: 1490–1496, 1993
Kakuta T, Currier JW, Haudenschild CC, Ryan TJ, Faxon DP: Differences in compensatory vessel enlargement, not intimal formation, account for restenosis after angioplasty in the hypercholestrolemic rabbit model. Circulation 89: 2809–2815, 1994
Glagov S, Weisenberg E, Zarins CK, Stankunavicius R, Kolettis GJ: Compensatory enlargement of human atherosclerotic coronary arteries. N Engl J Med 316: 1371–1375, 1987
Zarins CK, Zatina MA, Giddens DP, Ku DN, Glagov S: Shear stress regulation of artery lumen diameter in experimental atherogenesis. J Vasc Surg 5: 413–420, 1987
Spears JR, Serur J, Shrophire D, Paulin S: Fluorescence of experimental atheromatous plaques with hematoporphyrin derivative. J Clin Invest 71: 395–399, 1983
Figge FHJ, Weiland GS, Manganiello LOJ: Cancer detection and therapy: affinity of neoplastic, embryonic and traumatized tissue for porphyrins and metalloporphyrins. Proc Soc Exp Biol Med 68: 640–641, 1948
Litvack F, Grundfest WS, Forrester JS, Fishbein MC, Swan HJC, Corday E, Rider DM, McDermid IS, Pacala TJ, Laudenslager JB: Effects of hematoporphyrin derivative and photodynamic therapy on atherosclerotic rabbits. Am J Cardiol 56: 667–671, 1985
Spokojny AM, Serur JR, Skillman J, Spears JR: Uptake of hematoporphyrin derivative by atheromatous plaques: studies in human in vitro and rabbit in vivo. J Am Coll Cardiol 8: 1387–1392, 1986
Pollock ME, Eugene J, Hammer-Wilson M, Berns MW: Photosensitization of experimental atheromas by porphyrins. J Am Coll Cardiol 9: 639–646, 1987
Ortu P, LaMuraglia GM, Roberts WG, Flotte TJ, Hasan T: Photodynamic therapy of arteries: a novel approach for treatment of experimental intimal hyperplasia. Circulation 85: 1189–1196, 1992
Eton D, Colburn MD, Shim V, Panek W, Lee D, Moore WS, Alm SS: Inhibition of intimal hyperplasia by photodynamic therapy using Photofrin. J Surg Res 53: 558–562, 1992
Asahara T, Kato T, Amemiya T, Rakue H, Ooike Y, Shiraishi H, Usiu M, Oda Y, Naito Y, Ibukiyama C: In vivo experimental study on photodynamic therapy for the prevention of restenosis after angioplasty. Circulation 86 (suppl I): 1–846, 1992
LaMuraglia GM, ChandraSekar NR, Flotte TJ, Abbott WM, Michaud N, Hasan T: Photodynamic therapy inhibition of experimental intimal hyperplasia: acute and chronic effects. J Vasc Surg 19: 321–331, 1994
Nyameke I, Anglin S, McEwan J, MacRobert A, Bown S, Bishop C: Photodynamic therapy of normal and balloon-injured rat carotid arteries using 5-amino-levulinic acid. Circulation 91: 417–425, 1995
Dougherty TJ: Photodynamic therapy. Photochem Photobiol 58: 895–900, 1993
Foote CS: Definition of Type I and Type II photosensitized oxidation. Photochem Photobiol 54: 659, 1991
Gomer GJ, Ferrario A, Hayashi N, Rucker N, Szirth BC, Murphree AL: Molecular, cellular, and tissue responses following photodynamic therapy. Lasers Surg Med 8: 450–463, 1988
Okunaka T, Eckhauser ML, Kato H, Bomaminio A, Yamamoto H, Aizawa K, Sarasua MM, Koehler KA: Correlation between photodynamic efficacy of differing porphyrins and membrane partitioning behavior. Lasers Surg Med 12: 98–103, 1992
Kreimer-Birnbaum M: Modified porphyrins, chlorins, phthalocyanins, and purpurins: second-generation photosensitizers for photodynamic therapy. Sem Hematol 26: 157–173, 1989
Gomer CJ: Preclinical examination of first and second generation photosensitizers used in photodynamic therapy. Photochem Photobiol 54: 1093–1107, 1991
Spikes JD: Effects of photodynamic treatment on the thermal-mechanical properties of collagen (rat tail tendon). Photochem Photobiol 57 (suppl): 96S, 1993
Dartsch PC, Wunderlich K, Ben-Hur E: Aluminium phthalocyanines-induced photolysis of human vascular wall cells in culture and the effect of fluoride on photodynamic action. Coronary Artery Dis 5: 851–855, 1994
Fingar VH, Wieman TJ, Wiehle SA, Cerrito PB: The role of microvascular damage in photodynamic therapy: the effect of treatment on vessel constriction, permeability, and leucocyte adhesion. Cancer Res 52: 1914–1921, 1992
deVree WJA, Fontijne-Dorsman ANRD, Koster JF, Sluiter W: Photodynamic treatment of human endothelial cells promotes the adherence of neutrophils in vitro. Br J Cancer: in press, 1996
Gilissen MJ, van de Merbel-de Wit LEA, Star WM, Koster JF, Sluiter W: Effect of photodynamic therapy on the endothelial-dependent relaxation of isolated rat aortas. Cancer Res 53: 2548–2552, 1993
Zimmerman GA, Prescott SM, McIntyre TM: Endothelial cell interactions with granulocytes: tethering and signalling molecules. Immunol Today 13: 93–100, 1992
Foster TH, Primavera MC, Marder VJ, Hilf R, Sporn LA: Photosensitized release of von Willebrand factor from cultured human endothelial cells. Cancer Res 51: 3261–3266, 1991
Hattori R, Hamilton KK, McEver RP, Sims PJ: Complement proteins C5b-9 induce secretion of high molecular weight multimer of endothelial von Willebrand factor and translocation of granule membrane protein GMP-140 to the cell surface. J Biol Chem 264: 9053–9060, 1989
Libby P, Schwartz D, Brogi E, Tanaka H, Clinton SK: A cascade model for restenosis. A special case of atherosclerosis progression. Circulation 86(suppl III): 11147–11152, 1992
Hansen PR: Role of neutrophils in myocardial ischemia and reperfusion. Circulation 91: 1872–1885, 1995
Pietersma A, Kofflard M, De Wit LEA, Stijnen Th, Koster JF, Serruys PW, Sluiter W: Late lumen loss after coronary angioplasty is associated with the activation status of circulating phagocytes before treatment. Circulation 91: 1320–1325, 1995
Santamaria P, Gehrz RC, Bryan MK, Barbosa JJ: Involvement of class II MHC molecules in the LPS-induction of IL-1/TNF secretions by human monocytes: quantitative differences at the polymorphic level. J Immunol 143: 913–922, 1989
Hayes MP, Zoon KC: Priming of human monocytes for enhanced lipopolysaccharideresponses: expression of alpha interferon, interferon gamma, and tumor necrosis factor. Infect Immun 61: 3222–3227, 1993
Kuijpers TW, Hoogerwerf M, van der Laan LJ, Nagel G, van der Schoot CE, Grunert F, Roos D: CD66 nonspecific cross-reacting antigens are involved in neutrophil adherence to cytokine-activated endothelial cells. J Cell Biol 118: 457–466, 1992
Buchanan MR: Inhibition of thrombosis by leukocytes: role of endogenous fatty acid metabolites. Sanofi Foundation Thromb Res Bull 4: 14–22, 1989
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Sluiter, W., de Vree, W.J.A., Pietersma, A. et al. Prevention of late lumen loss after coronary angioplasty by photodynamic therapy: Role of activated neutrophils. Mol Cell Biochem 157, 233–238 (1996). https://doi.org/10.1007/BF00227904
Issue Date:
DOI: https://doi.org/10.1007/BF00227904