Abstract
Several anesthetics have been reported to suppress the transcription of a number of genes, including Arc, also known as Arg3.1, an immediate early gene that plays a significant role in memory consolidation. The purpose of this study was to explore the mechanism of anesthesia-mediated depression in Arc gene and protein expression. Here, we demonstrate that isoflurane or propofol anesthesia decreases hippocampal Arc protein expression in rats and mice. Surprisingly, this change was secondary to anesthesia-induced hypothermia. Furthermore, we confirm in vivo and in vitro that hypothermia per se is directly responsible for decreased Arc protein levels. This effect was the result of the decline of Arc mRNA basal levels following inhibition of ERK/MAPK by hypothermia. Overall, our results suggest that anesthesia-induced hypothermia leads to ERK inhibition, which in turns decreases Arc levels. These data give new mechanistic insights on the regulation of immediate early genes by anesthesia and hypothermia.
Similar content being viewed by others
Introduction
Synaptic plasticity plays a pivotal role in memory formation and is a process dependent on rapid changes in gene expression. The mRNA of the immediate early gene Arc (Activity-regulated cytoskeleton-associated protein), also known as Arg3.1, is rapidly transported to dendritic segments, where subsequent Arc protein synthesis at synapses appears to play a significant role in the neuronal plasticity associated with learning and memory1. Indeed, studies have demonstrated that the disruption or suppression of Arc gene expression impairs the maintenance of long-term potentiation2 as well as the consolidation of synaptic plasticity and memory3,4.
Volatile anesthetics have been reported to suppress the transcription of a number of genes, including Arc5,6. Furthermore, amnestic doses of the commonly used intravenous anesthetic, propofol, have been demonstrated to decrease Arc protein levels7. However, the mechanism underlying Arc depression by anesthesia is still unknown. Thus, despite neurobehavioral evidence that anesthetics impair memory and learning8,9, there is limited mechanistic information regarding how Arc gene and protein expression are altered by clinically relevant doses of anesthetics that are capable of producing surgical anesthesia.
Here, we hypothesized that exposure to clinically relevant doses of volatile or intravenous anesthetics would lead to a decrease in Arc protein levels by altering Arc translation and/or transcription. We found that Arc protein and mRNA expression were downregulated during isoflurane anesthesia. Surprisingly, this was not mediated by the exposure to isoflurane per se, but to the hypothermia consequent to anesthesia. We also showed that this effect was not due to a down-regulation of Arc translation by eukaryotic elongation factor 2 (eEF2), but a result of the decline of Arc mRNA basal levels following inhibition of Extracellular signal-Regulated Kinase/Mitogen-Activated Protein Kinase (ERK/MAPK) by hypothermia. We also confirmed that ERK inhibition is sufficient to decrease basal Arc protein levels by demonstrating that genetic ablation of MEK1 (MAPK/ERK Kinase 1, also known as MAPKK1), the kinase upstream of ERK, leads to decreases in phospho-ERK and Arc protein levels in the mouse hippocampus. Lastly, we verified our findings with propofol (an intravenous anesthetic) and exposure to hypothermia and confirmed low temperatures were directly responsible for the Arc protein decrease, through an effect on ERK activation and subsequent Arc gene transcription.
Results
Isoflurane-induced hypothermia mediates an immediate decrease in Arc protein levels in rats
Isoflurane is a halogenated ether commonly used for inhalational anesthesia in humans and animals. The rats were exposed to 1 minimum alveolar concentration (1 MAC = 1.3%) isoflurane, a clinically relevant dose that allows spontaneous ventilation10 and does not significantly alter hemodynamic parameters in rodents with or without temperature maintainance11,12,13. The mean rectal temperatures are summarized for all groups of rats in Supplementary Table 1. Without a warming device, significant hypothermia (29.0 ± 1.5°C, n = 8) occurred at the end of isoflurane administration (IH groups). In the groups under normothermic conditions, there was no significant decrease in body temperature (IN groups).
We then analyzed hippocampal Arc levels since Arc expression in the hippocampus plays an important role the formation of long-term memory3,4. Under hypothermic conditions, anesthesia with 1 MAC isoflurane for 3 hours led to a decrease in Arc protein levels to ~65% of controls (Fig. 1A1; Ctl vs. IH). However, this decrease was transient, as Arc protein levels were not significantly different from the control group after 24 h (Fig. 1A1; Ctl vs. IH24h). There was no variation in β-actin levels in all the experimental conditions (Fig. 1A2 & 1B2). Interestingly, the maintenance of normothermia during isoflurane administration prevented the decrease in Arc protein levels observed under hypothermic conditions (Fig. 1B1; Ctl vs. IN). Our results demonstrate that Arc protein levels decrease rapidly during anesthesia; however, this reduction was surprisingly not due to isoflurane per se, but was mediated by isoflurane-induced hypothermia.
Effect of isoflurane anesthesia on Arc protein levels in rats.
Hippocampal Arc (1) and β-actin (2) proteins immunoblot relative band intensity (expressed as % of control) in Fischer 344 rats following exposure to isoflurane under hypothermic conditions (A) or normothermic conditions (B). Hippocampal tissues were sampled immediately at the end of anesthesia (IH: Isoflurane-Hypothermia and IN: Isoflurane-Normothermia), or 24 h later (IH24h: Isoflurane-Hypothermia 24h and IN24h: Isoflurane-Normothermia 24h). One lane from representative immunoblots for Arc and β-actin are displayed for each condition. Dividing lines represent areas where lanes from the same blot were removed and the remaining lanes were spliced together. Original unaltered data from two batches of Fisher 344 rats can be found in Fig. S1. Data are expressed as mean ± SD, ** symbol denotes a significant difference versus control with P < 0.01, n = 8 for all conditions.
The reduction in Arc protein levels is not due to the modulation of Arc translation by eEF2 in rats
Arc protein levels are controlled at the translation level by eukaryotic elongation factor 2 (eEF2), an essential factor for protein synthesis. The activity of eEF2 is regulated by phosphorylation at Thr56 that inhibits its activity14, but is associated with an increase in Arc translation1,15,16. Therefore, we next determined whether the decrease in Arc protein levels observed in the presence of isoflurane-induced hypothermia was due to a change in Arc translation mediated by the phosphorylation/activation of eEF2. There was a ~200% transient increase in phospho-eEF2 levels under hypothermic conditions (Fig. 2A1, Ctl vs. IH); however, no significant change occurred when the rats temperature was maintained at 37°C (Fig. 2B1, Ctl vs. IN). Moreover, phospho-eEF2 levels returned to control levels 24 hours after anesthesia, when normothermia was restored (Fig. 2A1 Ctl vs. IH24h). Protein levels of total eEF2 did not change during anesthesia, neither under hypothermic nor normothermic conditions (Fig. 2A2, Ctl vs. IH; Fig. 2B2, Ctl vs. IN), but increased by 25~30% 24 h later, suggesting a delayed, temperature-independent effect of isoflurane anesthesia on eEF2 levels (Fig. 2A2, Ctl vs. IH24h; Fig. 2B2, Ctl vs. IN24h). Because an elevation of eEF2 phosphorylation at Thr56 should lead to an increase in Arc translation and Arc protein levels, our results suggest that reductions in Arc levels during hypothermia are not due to a modulation of Arc translation by eEF2.
Effect of isoflurane anesthesia on eEF2 and phospho-eEF2 protein levels in rats.
Hippocampal phospho-eEF2 (1) and eEF2 (2) protein immunoblot relative band intensity (% of control) in Fischer 344 rats following exposure to isoflurane under hypothermic conditions (A) or normothermic conditions (B). Hippocampal tissues were sampled immediately at the end of anesthesia (IH: Isoflurane-Hypothermia and IN: Isoflurane-Normothermia), or 24 h later (IH24h: Isoflurane-Hypothermia 24h and IN24h: Isoflurane-Normothermia 24h). One lane from representative immunoblots for phospho-eEF2 and eEF2 are displayed for each condition. Dividing lines represent areas where lanes from the same blot were removed and the remaining lanes were spliced together. Original unaltered data from two batches of Fisher 344 rats can be found in Fig. S2. Data are expressed as mean ± SD, * and ** symbols denote a significant difference versus control with P < 0.05 and P < 0.01, respectively, n = 8 for all conditions.
Isoflurane-induced hypothermia mediates a decrease in Arc gene expression in rats
As it was unlikely that changes in Arc translation were the cause of Arc protein reduction, we next examined Arc gene expression. Our data revealed that hippocampal Arc mRNA levels significantly and transiently decreased to ~35% of control immediately at the end of isoflurane exposure (Fig. 3A, Ctl vs. IH). In contrast, in rats that received isoflurane anesthesia under normothermic conditions, there was no significant change in hippocampal Arc mRNA levels (Fig. 3B, Ctl vs. IN). Arc mRNA levels were restored to normal levels 24 hours after anesthesia when the animals were normothermic (Fig. 3A Ctl vs. IN24h). Hence, hippocampal Arc mRNA changes, following isoflurane anesthesia in IH and IN, paralleled changes in Arc protein levels at all time points. Our results demonstrate that Arc mRNA levels decrease rapidly during anesthesia; however, this reduction is not due to isoflurane per se, but rather mediated by isoflurane-induced hypothermia.
Effect of isoflurane anesthesia on Arc mRNA levels in rats.
Hippocampal Arc mRNA levels (normalized to β-actin mRNA and expressed as % of control) in Fischer 344 rats following exposure to isoflurane under hypothermic conditions (A) or normothermic conditions (B). Hippocampal tissues were sampled immediately at the end of anesthesia (IH: Isoflurane-Hypothermia and IN: Isoflurane-Normothermia), or 24 h later (IH24h: Isoflurane-Hypothermia 24h and IN24h: Isoflurane-Normothermia 24h). Data are expressed as mean ± SD, *** symbol denotes a significant difference versus control with P < 0.001, n = 8 for all conditions.
Isoflurane-induced hypothermia leads to inhibition of ERK in rats
As we showed that Arc mRNA levels were diminished following anesthesia-induced hypothermia, we next investigated the mechanism underlying this decrease. It is known that synaptic activity drives Arc transcription in an ERK-dependent manner17. We thus examined the activation of ERK to see whether it could explain the decreased Arc transcription. ERK is 2 proteins ERK1 (44 kDa) and ERK2 (42 kDa). Here we quantified ERK1 and ERK2 together. Hippocampal phospho-ERK was reduced to ~36% of control immediately at the end of isoflurane exposure (Fig. 4A1, Ctl vs. IH) but returned to control values 24 h later (Ctl vs. IH24h). In contrast, there was no decrease in phospho-ERK in normothermic conditions (Fig. 4B1). Isoflurane treatment did not affect total ERK after 3 h (Fig. 4A2, 4B2, IH and IN), but there was a slight increase 24 h after normothermic exposure (Fig. 4B2, Ctl vs. IN24h). Thus, our results suggest that the isoflurane-induced hypothermia inhibits Arc transcription by inhibiting ERK activation.
Effect of isoflurane anesthesia on ERK and phospho-ERK protein levels in rats.
Hippocampal phospho-ERK (1) and ERK (2) protein immunoblot relative band intensity (% of control) in Fischer 344 rats following exposure to isoflurane under hypothermic conditions (A) or normothermic conditions (B). Hippocampal tissues were sampled immediately at the end of anesthesia (IH: Isoflurane-Hypothermia and IN: Isoflurane-Normothermia), or 24 h later (IH24h: Isoflurane-Hypothermia 24h and IN24h: Isoflurane-Normothermia 24h). One lane from representative immunoblots for phospho-ERK and ERK are displayed for each condition. ERK1 (44 kDa) and ERK2 (42 kDa) were quantified together. Dividing lines represent areas where lanes from the same blot were removed and the remaining lanes were spliced together. Original unaltered data from two batches of Fisher 344 rats can be found in Fig. S4. Data are expressed as mean ± SD, * and ** symbols denote a significant difference versus control with P < 0.05 and P < 0.01, respectively, n = 8 for all conditions.
Hypothermia induced by non-volatile anesthetics also leads to the inhibition of ERK and an Arc protein decrease in mice
As we demonstrated that isoflurane-induced hypothermia led to decreased Arc mRNA and protein levels, to ERK inhibition as well as to eEF2 activation, we next wanted to verify whether these results were specific to isoflurane-induced hypothermia or could be replicated with another anesthetic inducing hypothermia. We chose to test the effect of propofol, an intravenous sedative-hypnotic commonly used as an anesthetic for procedures requiring general anesthesia or conscious sedation as well as for prolonged sedation in intensive care units18. Moreover, we wanted to determine whether these effects were specific to male animals, so we injected propofol in female mice at 250 mg/kg, a dose that maintains spontaneous ventilation in B6 mice19. One hour following the injection of propofol, the rectal temperature of the mice dropped significantly from 36.5 ± 0.3°C (n = 5) to 25.4 ± 2.3°C (n = 4). Arc protein (~70% of control, Fig. 5.1) and phospho-ERK (~20% of control, Fig. 5.5) levels decreased significantly. There was no decrease in ARC level after normothermic administration of propofol (data not shown). These results are consistent with the observations made in rats following isoflurane exposure and suggest that they are mediated by anesthetic-induced hypothermia and not consequent to hypothermia induced by a specific class of anesthetics.
Effect of propofol anesthesia on Arc, eEF2 and ERK proteins levels in mice.
Hippocampal Arc (1), β-actin (2), phospho-eEF2 (3), eEF2 (4), phospho-ERK (5) and ERK (6) protein immunoblot relative band intensity (% of control) in C57BL/6J mice following exposure to propofol under hypothermic conditions. Hippocampal tissues from the propofol-anesthetized mice were obtained immediately at the end of anesthesia (Prop). ERK1 (44 kDa) and ERK2 (42 kDa) were quantified together. Two lanes from representative immunoblots for all the proteins are displayed for each condition. Dividing lines represent areas where lanes from the same blot were removed and the remaining lanes were spliced together. Original unaltered data can be found in Fig. S5. Data are expressed as mean ± SD, * and *** symbols denote a significant difference versus control with P < 0.05 and P < 0.001, respectively, n = 5 for Ctl and 4 for Prop.
Hypothermia during cold water swimming leads to the inhibition of ERK and an Arc protein decrease in mice
Although our results strongly suggest that the decreases in ERK activation and Arc protein levels are due to anesthesia-induced hypothermia, they do not irrefutably prove that they are the consequence of hypothermia per se. To address this issue, we induced hypothermia in mice using the cold water swimming (CWS) method20, without any anesthetic or other pharmacological intervention. Thirty minutes after CWS, the mice rectal temperature dropped to 29.6 ± 1.7°C (n = 4); Arc protein (~53% of control, Fig. 6.1) and phospho-ERK (~72% of control, Fig. 6.5) levels decreased significantly. In summary, these results demonstrate that the activation of ERK and levels of Arc protein in vivo can be negatively affected by hypothermia.
Effect of cold water swimming on Arc, eEF2 and ERK proteins levels in mice.
Hippocampal Arc (1), β-actin (2), phospho-eEF2 (3), eEF2 (4), phospho-ERK (5) and ERK (6) protein immunoblot relative band intensity (% of control) in C57BL/6J mice following cold water swimming (CWS). Hippocampal tissues from mice were obtained 30 min after CWS. ERK1 (44 kDa) and ERK2 (42 kDa) were quantified together. Two lanes from representative immunoblots for all the proteins are displayed for each condition. Dividing lines represent areas where lanes from the same blot were removed and the remaining lanes were spliced together. Original unaltered data can be found in Fig. S6. Data are expressed as mean ± SD, * symbol denotes a significant difference versus control with P < 0.05, n = 4 for all conditions.
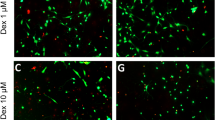
Hypothermia leads to the inhibition of ERK and an Arc protein decrease in SH-SY5Y cells
We next wanted to determine whether hypothermia also mediated its effects on Arc protein levels and ERK activation in vitro. We chose SH-SY5Y human neuroblastoma cells for this experiment as they are known to express Arc protein21. Two hours following incubation at 30°C, there was a significant decrease in Arc (~58% of control, Fig. 7.1) and phospho-ERK (~29% of control, Fig. 7.5) protein levels, while eEF2 and total ERK protein levels did not change (Fig. 7.4 and 7.6, respectively, n = 6).
Effect of hypothermia on Arc, eEF2 and ERK proteins levels in SH-SY5Y cells.
Arc (1), β-actin (2), phospho-eEF2 (3), eEF2 (4), phospho-ERK (5) and ERK (6) protein immunoblot relative band intensity (% of control) in SH-SY5Y cells following exposure to hypothermic conditions. Cell lysates were sampled immediately at the end of 2 hours culture at 37°C (Ctl) or 30°C (Hypo). ERK1 (44 kDa) and ERK2 (42 kDa) were quantified together. Three lanes from representative immunoblots for all the proteins are displayed for each condition. Original unaltered data from two batches of SH-SY5Y cells can be found in Fig. S7a and S7b. Data are expressed as mean ± SD, * and *** symbols denote a significant difference versus control with P < 0.05 and P < 0.001, respectively, n = 6 for all conditions.
Suppression of ERK activity by deletion of MAPK/ERK Kinase 1 (Mek1) leads to an Arc protein decrease in mice
All our results thus far demonstrate that hypothermia leads to the inhibition of ERK and a decrease in basal Arc protein levels both in vivo and in vitro. However, these results are only correlative and do not prove that the decrease in phospho-ERK is responsible for the down-regulation of Arc. To provide additional evidence that ERK inactivation is directly responsible for the decreased Arc protein levels, we used mice without MEK1 and MEK2, the upstream kinases activating ERK. Mek2−/− mice are straight knockout mice that are viable, but do not display any effect on ERK phosphorylation, probably because of a rescue by MEK122. They are used here as negative controls. Ablation of Mek1 is lethal during embryonic development, not because of an effect in the embryos, but because of its impact on placental angiogenesis23. To circumvent this limitation, we used Mek1−/− conditional knockout mice that excise Mek1 only in the embryos. These mice are viable and have a marked decrease in ERK phosphorylation24. Deletion of Mek1 decreased phospho-ERK to ~24% of control and Arc protein levels to ~48% of control (Fig. 8.1 & 8.5, respectively), but there was no change in either actin, eEF2, phospho-eEF2 or total ERK (Fig. 8). Deletion of Mek2 had no effect on any of the proteins studied here (Fig. 8). These results demonstrate that inhibition of ERK is sufficient to lead to decreased Arc protein levels.
Effect of Mek1 and Mek2 gene deletion on Arc, eEF2 and ERK protein levels in mice.
Hippocampal Arc (1), β-actin (2), phospho-eEF2 (3), eEF2 (4), phospho-ERK (5) and ERK (6) protein immunoblot relative band intensity (% of control) in Mek1−/− and Mek2−/− mice. ERK1 (44 kDa) and ERK2 (42 kDa) were quantified together. Two lanes from representative immunoblots for all the proteins are displayed for each condition. Original unaltered data can be found in Fig. S8. Data are expressed as mean ± SD, ** and *** symbols denote a significant difference versus control with P < 0.01 and P < 0.001, respectively, n = 4 for all conditions.
Overall, our results, both in vivo and in vitro, demonstrate that the decrease in Arc and phospho-ERK protein levels during the administration of anesthesia, without control of temperature, are secondary to the direct effect of hypothermia, Furthermore, the inhibition of ERK is sufficient to induce a decrease in Arc protein levels.
Discussion
In the current study, we explored the mechanisms involved in anesthesia-mediated depression of Arc gene and protein expression. We demonstrate that it is not due to the anesthetics per se, but the result of hypothermia. The effect of hypothermia in animals was very robust and reproducible i) in different species (rats or mice), ii) in males or females, iii) with different inducers of hypothermia (isoflurane, propofol, or cold-water swimming), iv) at different temperatures, v) and with different times of exposure. Importantly, Arc expression was also diminished in SH-SY5Y cells after direct exposure to hypothermia.
As anesthesia-induced hypothermia resulted in reduction of Arc protein levels, we initially investigated the molecular mechanism of this decrease by examining the phosphorylation of eEF2 protein, which regulates Arc translation. Normally, increased phospho-eEF2 should lead to enhanced Arc translation1,15. Surprisingly, the reduction in Arc protein correlated with an increased phosphorylation of eEF2, which suggests that eEF2-mediated control of translation is not involved in Arc protein decline during hypothermia. We also observed a robust decline in Arc mRNA levels, indicating that the fall in the Arc protein is due to inhibition of Arc transcription during anesthesia-induced hypothermia. Arc transcription can be regulated by ERK activity, where synaptic activity drives Arc transcription in an ERK-dependant manner17. Therefore, we investigated the levels of phospho-ERK and found a significant decrease during isoflurane-induced hypothermia. More importantly, the decrease in Arc protein and phospho-ERK were reproduced following hypothermia induced by propofol or cold-water swimming in mice as well as in SH-SY5Y cells incubated at 30°C, demonstrating a direct effect of low temperatures.
Interestingly, synaptic activity induces the phosphorylation of ERK resulting in increased Arc protein levels, while inhibitors of ERK activation block stimulus-induced Arc gene and protein expression1,25. However, it was not known whether a decrease in basal ERK activation could lead to a decrease in basal Arc protein levels. Here, we show that a reduction in basal ERK activation by hypothermia correlates with depressed Arc expression and we demonstrate that genetic reduction of ERK activation by ablation of MEK1 causes a decrease in basal Arc levels.
Overall, our results demonstrate that Arc protein and mRNA are decreased as a direct consequence of hypothermia, both in vivo and in vitro. They also suggest that hypothermia mediates its effects on Arc protein levels through inhibition of ERK.
Part of our data confirm and extend previous results showing that exposure to sevoflurane, another fluorinated hydrocarbon volatile anesthetic, leads to an immediate and persistent decrease in Arc mRNA in the rat brain5. However, in contrast to that study, the inhibitory effect of anesthesia on Arc mRNA observed in the present study was transient, returning to normal levels 24 h after isoflurane exposure. One explanation might be that these investigators did not report the temperature of the rats and used sevoflurane at 4%, which corresponds to a value as high as approximately 1.7 MAC in this species26,27, in contrast to the 1 MAC isoflurane used in the present study. Furthermore, hypoxia, which commonly occurs at these higher anesthetic doses, has been demonstrated to significantly alter immediate-early gene expression28. Hence, while the distinct possibility exists that transient versus persistent changes in Arc mRNA could be explained by a dose dependent phenomenon, it is also possible that at higher anesthetic concentrations, they are secondary to anesthetic-induced physiologic perturbations. Indeed, Kobayashi et al. observed that a dose of 4.5% sevoflurane, which is slightly higher than the final concentration used in their study (4%), resulted in death in some of their animals due to hypoxia or hypotension5.
Hypothermia has been previously demonstrated to either increase or decrease the expression of certain immediate early genes such as c-fos, fosB, fra-1, fra-2, c-jun and junB, following an ischemic insult in the rat forebrain29. Interestingly, in terms of Arc, Otsuka et al. demonstrated that following transient global ischemia in normothermic mice, there was a persistent increase in hippocampal Arc transcription that was absent in hypothermic mice30. Although we did not examine Arc expression in the context of ischemia, our findings of a suppressant effect of hypothermia on Arc gene and protein expression are indeed consistent with those of Otsuka et al. and they demonstrate that hypothermia is a potent inhibitor of Arc expression, even in the setting of conditions not specifically associated with induced Arc expression.
Hypothermia has been known for a long time to lead to memory disruption in numerous organisms including rodents31. In rats, memory loss has been demonstrated after cooling31,32,33,34. However, the mechanisms by which hypothermia produces memory disruption are not well understood. Some studies suggest that a reduction of protein synthesis resulting from a general decrease in energy-dependent cellular processes plays a role, whereas others suggest a disruption of cellular signaling events positioned upstream of transcription or translation35. Our results demonstrating a decrease in Arc protein and mRNA levels correlating with decreased ERK signaling following hypothermia argue for the latter hypothesis and provide a clue to a possible mechanism underlying the disruption of memory following cooling in wide range of organisms. While it is outside of the scope of this article to test the physiological consequences of our observations, our results suggest that future studies are warranted to specifically determine whether changes in Arc gene and protein expression following anesthesia or other initiators of perioperative temperature loss contribute directly to the impairment of mnemonic function.
Another potentially memory altering event occuring during hypothermic anesthesia is the hyperphosphorylation of tau19,36,37, a microtubule associated protein implicated in many neurodegenerative diseases, including Alzheimer's38,39. Tau hyperphosphorylation and/or aggregation is thought to contribute to memory deficits40. Hence, it would be interesting to dissect the respective roles of hypothermia, Arc and tau proteins in memnotic impairment following anesthesia by using tau knock-out mice.
Although it would be premature to clinically extrapolate the results of the current study to the clinical arena, the finding that anesthesia-induced hypothermia accounts for a significant change in a protein associated with memory consolidation is potentially relevant, as the perioperative occurrence of cognitive impairment41 and hypothermia42 following general anesthesia are quite common.
In summary, we conclude that anesthesia-induced hypothermia has profound effects on Arc gene expression and protein synthesis in the hippocampus and that this effect is probably mediated through inhibition of ERK signaling. These data give novel mechanistic insights on the regulation of immediate early genes by anesthesia and hypothermia. The current study may also have significant implications for the interpretation of data from studies that have examined Arc activation in anesthetized animals without the control of body temperature.
Methods
Animals and treatments
12–16-week-old Fischer 344 rats (Taconic, Germantown, NY) or 12-week-old C57BL/6J mice (The Jackson Laboratory, Bar Harbor, ME) were housed at 22°C and were kept on a 12 h/12 h light/dark cycle. All animals had access to food and water ad libitum. The experimental protocols were approved by the Columbia University Animal Care and Use Committee or the Comité de Protection des Animaux du Centre Hospitalier de l'Université Laval and, in accordance with NIH (National Institutes of Health) and CIHR (Canadian Institutes for Health Research) guidelines, adequate measures were taken to minimize pain and discomfort.
During the isoflurane (2-chloro-2-(difluoromethoxy)-1,1,1-trifluoro-ethane) anesthesia studies, male rats received either isoflurane (Abbott Laboratories, Chicago, Il) at 1 MAC (1.3%) in a 30% O2 in air mixture or a 30% O2 in air mixture alone (control) for a period of 3 h. In the hypothermia studies, the temperature of the rats was not controlled during anesthesia and was allowed to spontaneously decrease. In the normothermia studies, rats exposed to isoflurane were anesthetized in a warmed Plexiglas anesthesia chamber equipped with a heating pad and lamps to maintain the rectal temperature at 37°C. Isoflurane and O2 concentrations in the chamber were determined using a respiratory gas monitor (Ohmeda 5250 RGM, Datex-Ohmeda, Louisville, CO) and spontaneous ventilation was maintained throughout the entire study. The rats were killed using decapitation either immediately following isoflurane exposure (IH and IN groups for Isoflurane Hypothermia and Isoflurane Normothermia, respectively) or 24 h after (IH24 and IN24 groups for Isoflurane Hypothermia after 24 h and Isoflurane Normothermia after 24 h, respectively).
For propofol (2,6 diisopropylphenol) anesthesia, a 25 mg/ml solution of propofol (MP Biomedicals, Solon, OH) in intralipid (20% fat emulsion) was freshly prepared. Female mice were treated with either propofol (MP Biomedicals, Solon, OH) 250 mg/kg or an equivalent volume of intralipid (vehicle control for propofol, Sigma RBI, St. Louis, MO) via intraperitoneal (i.p.) injection and anesthesia was assessed as loss of righting reflex. The dose of propofol was choosen according to our previous study19. One hour after injection, the mice were killed by decapitation.
Cold Water Swimming (CWS) experiments were conducted as previously described20. Briefly, mice swam in ice-cold water for 5 min, after which they were gently wiped dry and returned to their cages for 30 min. The temperature of the mice after CWS is ~16°C and ~25°C 30 min. later43. Control animals swam for 5 min. in warm water, which keeps their temperature around 37°C43. Mice were killed by decapitation 30 min after CWS.
For experiments with mice lacking MEK1 or MEK2, which are the kinases upstream of ERK, we used Mek1−/− and Mek2−/− mice of either sex at 6.1 ± 2.0 month of age. Mek2−/− mice are straight knock-out mice22, while Mek1−/− mice are conditional knockout mice that excise Mek1 during embryonic development24 to avoid placental lethality23.
For all the experiments, rectal temperature was monitored with a digital thermometer (Thermalert TH-5, Physiotemp, Clifton, NJ). After decapitation, hippocampal tissue was dissected, immediately frozen on liquid nitrogen or dry ice and then stored at −80°C. Protein extraction from frozen samples was performed as previously described44.
All animals were handled according to procedures approved by the Columbia University Animal Care and Use Committee in accordance with National Institutes of Health (NIH) guidelines, or by the Comité de Protection des Animaux du CHUQ under the guidelines of the Canadian Council on Animal Care. Adequate measures were taken to minimize pain and discomfort.
Cell experiments
SH-SY5Y cells (ATCC #CRL-2266, American Type Culture Collection, Manassas, VA) were maintained, as recommended by the provider, in a 1:1 mixture of ATCC-formulated Eagle's Minimum Essential Medium and F12 Medium, in a 5% CO2 humidified incubator at 37°C. For hypothermia exposure, cells were placed in a 5% CO2 humidified incubator at 30°C for 2 hours, as described19. Cells were washed in cold phosphate buffered saline and harvested in a modified RIPA (radioimmunoprecipitation assay) buffer as described45. Total protein concentration was determined by the BCA (bicinchoninic acid) Protein Assay (Pierce Biotechnology, Rockford, IL) and samples were processed for Western blotting as described below.
Protein immunoblot detection
SDS-PAGE and Western blot analyses were performed as described previously37, using the following primary antibodies: Arc mouse monoclonal clone C-7 (sc-17839, 1:200 dilution, Santa Cruz Biotechnology, Santa Cruz, CA) or clone 40 (#612603, 1:1000 dilution, BD Transduction Laboratories, Franklin Lakes, NJ), anti-β-Actin monoclonal (clone AC-74, 1:5000 dilution, Sigma), eukaryotic elongation factor (eEF2) polyclonal (#2332, 1:1000 dilution, Cell Signaling Technology, Danvers, MA), phospho-eEF2 rabbit polyclonal (Thr56, #2331, 1:1000, Cell Signaling), ERK/MAPK rabbit polyclonal (p44/42 MAPK, #9102, 1:1000, Cell Signaling) and p-ERK rabbit polyclonal (Phospho-p44/42 MAPK Thr202/Tyr204, #9101, 1:1000, Cell Signaling). Immunoreactive bands were analyzed using a Fujifilm LAS-4000 imaging system and ImageGauge image analysis software (Version 4.2, Fujifilm USA, Valhalla, NY).
RNA extraction and real-time quantitative polymerase chain reaction analysis
Total RNA was extracted using TRIZOL reagent (Invitrogen Corporation, Carlsbad, CA). The PureLink RNA Mini Kit (Invitrogen) with on-column PureLink DNase treatment (Invitrogen) was used for the purification of the total RNA according to the manufacturer's protocol. One μg of RNA was reverse-transcribed into cDNA using the SuperScript III First-Strand Synthesis Supermix for qRT-PCR (Invitrogen) according to the manufacturer's instructions.
Quantitative PCR amplification was carried out in a Bio-Rad iQ5 cycler (Bio-Rad Laboratories, Hercules, CA), using 5 μL of diluted cDNA (1:20 dilution), 500 nM concentration of the Arc primers, 250 nM concentration of the β-actin primers and iQ SYBR Green Supermix (Bio-Rad Laboratories, Hercules, CA) in a total volume of 20 μL. Arc46 and β-actin47 primer sequences were based on previous publications.
Statistical analysis
Group comparisons were made using one-way ANOVA with Bonferroni's post-hoc test, or a Student t-test using Prism 4 statistical analysis software (GraphPad Software, San Diego, CA) on a MacBook Pro. All data are reported as mean ± SD and a value of P < 0.05 was considered statistically significant.
References
Bramham, C. R., Worley, P. F., Moore, M. J. & Guzowski, J. F. The immediate early gene arc/arg3.1: regulation, mechanisms and function. J Neurosci 28, 11760–11767 (2008).
Messaoudi, E. et al. Sustained Arc/Arg3.1 synthesis controls long-term potentiation consolidation through regulation of local actin polymerization in the dentate gyrus in vivo. J Neurosci 27, 10445–10455 (2007).
Guzowski, J. F. et al. Inhibition of activity-dependent arc protein expression in the rat hippocampus impairs the maintenance of long-term potentiation and the consolidation of long-term memory. J Neurosci 20, 3993–4001 (2000).
Plath, N. et al. Arc/Arg3.1 is essential for the consolidation of synaptic plasticity and memories. Neuron 52, 437–444 (2006).
Kobayashi, K., Takemori, K. & Sakamoto, A. Circadian gene expression is suppressed during sevoflurane anesthesia and the suppression persists after awakening. Brain research 1185, 1–7 (2007).
Sakamoto, A. et al. Influence of inhalation anesthesia assessed by comprehensive gene expression profiling. Gene 356, 39–48 (2005).
Ren, Y., Zhang, F. J., Xue, Q. S., Zhao, X. & Yu, B. W. Bilateral inhibition of gamma-aminobutyric acid type A receptor function within the basolateral amygdala blocked propofol-induced amnesia and activity-regulated cytoskeletal protein expression inhibition in the hippocampus. Anesthesiology 109, 775–781 (2008).
Culley, D. J., Baxter, M., Yukhananov, R. & Crosby, G. The memory effects of general anesthesia persist for weeks in young and aged rats. Anesthesia and analgesia 96, 1004–1009 (2003).
Culley, D. J., Baxter, M. G., Crosby, C. A., Yukhananov, R. & Crosby, G. Impaired acquisition of spatial memory 2 weeks after isoflurane and isoflurane-nitrous oxide anesthesia in aged rats. Anesthesia and analgesia 99, 1393–1397 (2004).
Whittington, R. A. & Virag, L. Isoflurane decreases extracellular serotonin in the mouse hippocampus. Anesthesia and analgesia 103, 92–98 (2006).
Redel, A. et al. Comparison of isoflurane-, sevoflurane- and desflurane-induced pre- and postconditioning against myocardial infarction in mice in vivo. Exp Biol Med (Maywood) 234, 1186–1191 (2009).
Menuet, C. et al. Isoflurane anesthesia precipitates tauopathy and upper airways dysfunction in pre-symptomatic Tau. P301L mice: possible implication for neurodegenerative diseases. Neurobiology of disease 46, 234–243 (2012).
Xie, Z. et al. The common inhalation anesthetic isoflurane induces caspase activation and increases amyloid beta-protein level in vivo. Annals of neurology 64, 618–627 (2008).
Redpath, N. T., Price, N. T., Severinov, K. V. & Proud, C. G. Regulation of elongation factor-2 by multisite phosphorylation. Eur J Biochem 213, 689–699 (1993).
Chotiner, J. K., Khorasani, H., Nairn, A. C., O'Dell, T. J. & Watson, J. B. Adenylyl cyclase-dependent form of chemical long-term potentiation triggers translational regulation at the elongation step. Neuroscience 116, 743–752 (2003).
Kanhema, T. et al. Dual regulation of translation initiation and peptide chain elongation during BDNF-induced LTP in vivo: evidence for compartment-specific translation control. Journal of neurochemistry 99, 1328–1337 (2006).
Pintchovski, S. A., Peebles, C. L., Kim, H. J., Verdin, E. & Finkbeiner, S. The serum response factor and a putative novel transcription factor regulate expression of the immediate-early gene Arc/Arg3.1 in neurons. J Neurosci 29, 1525–1537 (2009).
Wunsch, H., Kahn, J. M., Kramer, A. A. & Rubenfeld, G. D. Use of intravenous infusion sedation among mechanically ventilated patients in the United States. Crit Care Med 37, 3031–3039 (2009).
Whittington, R. A. et al. Propofol directly increases tau phosphorylation. PLoS ONE 6, e16648 (2011).
Okawa, Y., Ishiguro, K. & Fujita, S. C. Stress-induced hyperphosphorylation of tau in the mouse brain. FEBS Lett 535, 183–189 (2003).
Kremerskothen, J., Wendholt, D., Teber, I. & Barnekow, A. Insulin-induced expression of the activity-regulated cytoskeleton-associated gene (ARC) in human neuroblastoma cells requires p21(ras), mitogen-activated protein kinase/extracellular regulated kinase and src tyrosine kinases but is protein kinase C-independent. Neurosci Lett 321, 153–156 (2002).
Belanger, L. F. et al. Mek2 is dispensable for mouse growth and development. Mol Cell Biol 23, 4778–4787 (2003).
Giroux, S. et al. Embryonic death of Mek1-deficient mice reveals a role for this kinase in angiogenesis in the labyrinthine region of the placenta. Curr Biol 9, 369–372 (1999).
Bissonauth, V., Roy, S., Gravel, M., Guillemette, S. & Charron, J. Requirement for Map2k1 (Mek1) in extra-embryonic ectoderm during placentogenesis. Development 133, 3429–3440 (2006).
Rao, V. R. et al. AMPA receptors regulate transcription of the plasticity-related immediate-early gene Arc. Nat Neurosci 9, 887–895 (2006).
Crawford, M. W. et al. Haemodynamic and organ blood flow responses to sevoflurane during spontaneous ventilation in the rat: a dose-response study. Can J Anaesth 39, 270–276 (1992).
Crawford, M. W., Lerman, J., Saldivia, V. & Carmichael, F. J. Hemodynamic and organ blood flow responses to halothane and sevoflurane anesthesia during spontaneous ventilation. Anesthesia and analgesia 75, 1000–1006 (1992).
Nanduri, J., Yuan, G., Kumar, G. K., Semenza, G. L. & Prabhakar, N. R. Transcriptional responses to intermittent hypoxia. Respir Physiol Neurobiol 164, 277–281 (2008).
Kamme, F., Campbell, K. & Wieloch, T. Biphasic expression of the fos and jun families of transcription factors following transient forebrain ischaemia in the rat. Effect of hypothermia. Eur J Neurosci 7, 2007–2016 (1995).
Otsuka, N. et al. Transcriptional induction and translational inhibition of Arc and Cugbp2 in mice hippocampus after transient global ischemia under normothermic condition. Brain research 1287, 136–145 (2009).
Riccio, D. C., Hodges, L. A. & Randall, P. K. Retrograde amnesia produced by hypothermia in rats. J Comp Physiol Psychol 66, 618–622 (1968).
Hamm, R. J. Hypothermia-induced retrograde amnesia in mature and aged rats. Dev Psychobiol 14, 357–364 (1981).
Richardson, R., Riccio, D. C. & Morilak, D. Anterograde memory loss induced by hypothermia in rats. Behav Neural Biol 37, 76–88 (1983).
Santucci, A. C., Kasenow, P. M., Riccio, D. C. & Richardson, R. Hypothermia-induced anterograde amnesia: is memory loss attributable to impaired acquisition? Behav Neural Biol 48, 13–23 (1987).
Fulton, D., Kemenes, I., Andrew, R. J. & Benjamin, P. R. Time-window for sensitivity to cooling distinguishes the effects of hypothermia and protein synthesis inhibition on the consolidation of long-term memory. Neurobiol Learn Mem 90, 651–654 (2008).
Planel, E. et al. Anesthesia leads to tau hyperphosphorylation through inhibition of phosphatase activity by hypothermia. J Neurosci 27, 3090–3097 (2007).
Planel, E. et al. Anesthesia-induced hyperphosphorylation detaches 3-repeat tau from microtubules without affecting their stability in vivo. J Neurosci 28, 12798–12807 (2008).
Avila, J., Lucas, J. J., Perez, M. & Hernandez, F. Role of tau protein in both physiological and pathological conditions. Physiol Rev 84, 361–384 (2004).
Buee, L., Bussiere, T., Buee-Scherrer, V., Delacourte, A. & Hof, P. R. Tau protein isoforms, phosphorylation and role in neurodegenerative disorders. Brain Res. Brain. Res. Rev. 33, 95–130 (2000).
Duff, K. & Planel, E. Untangling memory deficits. Nat Med 11, 826–827 (2005).
Sauer, A. M., Kalkman, C. & van Dijk, D. Postoperative cognitive decline. J Anesth 23, 256–259 (2009).
Sessler, D. I. Temperature monitoring and perioperative thermoregulation. Anesthesiology 109, 318–338 (2008).
Planel, E. et al. Alterations in glucose metabolism induce hypothermia leading to tau hyperphosphorylation through differential inhibition of kinase and phosphatase activities: implications for Alzheimer's disease. J Neurosci 24, 2401–2411 (2004).
Planel, E. et al. Anesthesia leads to tau hyperphosphorylation through inhibition of phosphatase activity by hypothermia. J Neurosci 27, 3090–3097 (2007).
Tatebayashi, Y. et al. c-jun N-terminal kinase hyperphosphorylates R406W tau at the PHF-1 site during mitosis. Faseb J 20, 762–764 (2006).
Marie-Claire, C., Courtin, C., Roques, B. P. & Noble, F. Cytoskeletal genes regulation by chronic morphine treatment in rat striatum. Neuropsychopharmacology 29, 2208–2215 (2004).
Yasuda, M. et al. Robust stimulation of TrkB induces delayed increases in BDNF and Arc mRNA expressions in cultured rat cortical neurons via distinct mechanisms. Journal of neurochemistry 103, 626–636 (2007).
Acknowledgements
This work was supported by a National Institute of General Medical Sciences grants K08GM00681 and 1R01GM101698 (to R.A.W.), Biomedial Doctoral Awards from the Alzheimer Society of Canada (to N.B.E.K. and F.R.K.), grants from Canadian Institutes for Health Research (MOP-106423, PCN-102993), Natural Sciences and Engineering Research Council (354722), Canada Foundation for Innovation (23905) and a Research Scholar Career Awards (16205, 20048) from the Fonds de la Recherche en Santé du Québec (to E.P.). C.J. is supported by Postdoctoral Awards from the Alzheimer Society of Canada and the Alzheimer Society of Saskatchewan. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: R.A.W., E.P. Performed the experiments: A.B., L.V., T.O.M., F.M., C.J., N.B.E.K., F.M. Analyzed the Data: A.B., L.V., T.O.M., F.M., E.P. Contributed reagents/material/analysis tools: C.W.E., J.C. Wrote the manuscript: R.A.W., E.P. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Supplementary Information
Supplementary Information
Supplementary Information
Supplementary table 1
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Whittington, R., Bretteville, A., Virág, L. et al. Anesthesia-induced hypothermia mediates decreased ARC gene and protein expression through ERK/MAPK inactivation. Sci Rep 3, 1388 (2013). https://doi.org/10.1038/srep01388
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep01388
This article is cited by
-
Dexmedetomidine reduces propofol-induced hippocampal neuron injury by modulating the miR-377-5p/Arc pathway
BMC Pharmacology and Toxicology (2022)
-
Early life oxytocin treatment improves thermo-sensory reactivity and maternal behavior in neonates lacking the autism-associated gene Magel2
Neuropsychopharmacology (2022)
-
Anesthesia can alter the levels of corticosterone and the phosphorylation of signaling molecules
BMC Research Notes (2021)
-
Effects of hypothermia during propofol anesthesia on learning and memory ability and hippocampal apoptosis in neonatal rats
Journal of Anesthesia (2019)
-
Calcineurin/P-ERK/Egr-1 Pathway is Involved in Fear Memory Impairment after Isoflurane Exposure in Mice
Scientific Reports (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.