Abstract
We have investigated the crossing of the blood brain barrier (BBB) by the peptide gH625 and compared to the uptake by liver in vivo. We clearly observed that in vivo administration of gH625 allows the crossing of the BBB, although part of the peptide is sequestered by the liver. Furthermore, we used a combination of biophysical techniques to gain insight into the mechanism of interaction with model membranes mimicking the BBB and the liver. We observed a stronger interaction for membranes mimicking the BBB where gH625 clearly undergoes a change in secondary structure, indicating the key role of the structural change in the uptake mechanism. We report model studies on liposomes which can be exploited for the optimization of delivery tools.
Similar content being viewed by others
Introduction
Central nervous system (CNS) diseases constitute the largest area of unmet health demand; in fact, despite the presence of candidate therapeutic molecules, drug delivery is made difficult by the presence of the blood-brain barrier (BBB), which ultimately results in the limited entry of 95% of drug candidates which may be valuable for CNS diseases. The BBB is made by brain capillary endothelial cells closely interconnected with tight junctions which effectively seal the capillary wall eliminating any inter-endothelial space. In addition, there are efflux transporters which also play a key role in obstructing the entrance into the CNS1,2. Thus, crossing the BBB is a major challenge which has also been addressed by the use of nanosystems; although nanosystems may present several advantages for drug delivery in general, still the amount of drug that enters the brain is very low3,4. A key strategy to enhance brain delivery is represented by surface modification with ligand binding moieties or receptors expressed at the luminal surface of cerebral endothelial cells5. Two main processes have been put forward to elucidate the transport mechanism: receptor-mediated transcytosis (RMT) and adsorptive-mediated transcytosis (AMT)6,7.
Cell-penetrating peptides (CPPs) are short amphipathic and positively charged peptides acting as cargo carriers which enter complex physiological barriers without cell rupture thus in a non-invasive manner and without the aid of cell membrane receptors8. Although, evidences of the exact internalization mechanism are scarce and elusive, it has been commonly accepted that more than one mechanism may be involved7. Considering the major endocytic entry pathway, the general application of CPPs in drug delivery has been complicated by their entrapment in cellular organelles, which seriously reduces the cargo delivering efficacy.
Moreover, a current hotspot in CPP research is to understand whether their ability to cross the biological membranes also implies their ability to pass the BBB9. Although positively charged CPPs would be proper candidates to assist brain drug delivery via the AMT mechanism, scarce literature reports actually show their capacity to deliver cargoes through the BBB and often they result in divergent outcomes. As a matter of fact, a detailed overview with comparable, quantitative data of the currently available brain influx studies of CPPs is unavailable. Some authors showed that CPPs are able to reach the brain parenchyma both in vivo and in vitro10. In vivo evaluation of some CPP resulted in compromised BBB; as a matter of fact, although Tat-mediated delivery of neuroprotective drugs across the BBB in ischemia and seizure models were very promising, it was evidenced that the BBB was compromised9,11.
AMT delivery is triggered by electrostatic interactions between positive charges on the nanosystem and relative high concentration of negative charges on the membrane of brain endothelial cells7; however, positively charged particles often exhibit a rapid blood clearance together with aggregation problems and high accumulation in the lung and liver12. Therefore, the number and type of charges present on the surface of the nanosystem play a key role in CNS drug delivery.
In particular, the tissue distribution varies among the different CPPs, with most of them showing a higher liver distribution compared to other tissues, which can indicate metabolization, or uptake of the peptides and of their metabolites into hepatocytes9,13.
Considering that positively charged molecules may form aggregates in the presence of negatively charged serum proteins and result in enhanced accumulation in the lung and liver, less positive charged CPP may represent an alternative in order to achieve a more effective brain delivery. Recent progresses in the use of membranotropic peptides for the delivery of macromolecules across cell membranes, provide a great opportunity for CNS delivery14. These amphipathic peptides are capable of causing the membrane distortion necessary for insertion into the target membrane. Recently, the peptide gH625, belonging to this class of membranotropic sequences, showed remarkable vector properties, efficiently delivering a range of cargoes15. gH625 is essentially internalized by a non endocytic mechanism avoiding endosomal entrapment16,17,18,19,20,21,22,23 and is also shown to be able to cross the BBB in vitro and in vivo16,24. The peculiar ability of crossing physical barriers is probably correlated to the amino acid residues which seem to be central for the interaction and destabilization of the target lipid membranes; moreover, it is able to assume an amphipathic α-helical structure in membranes which is key to favouring the binding of proteins to membranes25. A mutagenesis study was done previously to understand the role of each residue in the peptide-lipid interaction, fusion and helix formation25,26,27,28.
In a previous work, gH625 was shown to be able to cross the BBB in vivo24. Uptake was not linked to alterations of cell viability or maximal mitochondrial oxidative capacity, suggesting that gH625 could potentially be used as a brain delivery system for macromolecules24. In general a high accumulation in the target tissue results in an improved therapeutic effect, while a large amount of drug distributed to non-target organs may cause unwanted toxicity and/or side effects. It is thus fundamental to reduce liver metabolism and renal clearance to produce prolonged blood circulation with an increased chance of accumulation in the target tissue12. Therefore, in order to employ gH625 as an attractive CPP for facilitating CNS delivery, it is fundamental to understand the affinity of the peptide for the BBB and for the liver. We started our analysis from in vivo bio-distribution analysis between BBB and liver and then using a combination of techniques and model membranes, we gained further insight into the mechanism of internalization which will help in the optimization of this and similar delivery tools.
Experimental Section
Materials
1-palmitoyl-2-oleoyl-sn-glycero-3-phosphocholine (POPC), dioleoyl phosphatidylcholine (DOPC), dioleoyl phosphatidylglycerol (DOPG), Sphingomyelin (SM), N-(7-nitro-benz-2-oxa-1,3-diazol-4-yl) phosphatidylethanolamine (NBD-PE) and N-(Lissamine-rhodamine-B-sulfonyl) phosphatidylethanolamine (Rho-PE) were purchased from Avanti Polar Lipids (Birmingham, AL, USA), while cholesterol (CHOL), Triton 100X and 4-chloro-7-nitrobenz-2-oxa-1,3-diazole (NBD-Cl) were purchased from Sigma (St. Louis, MO, USA). DAPI (4′,6-Diamidino-2-Phenylindole, Dilactate) was purchased from Invitrogen (Carlsbad, CA, USA), Sudan Black B from Sigma-Aldrich (St. Louis, MO, USA). Picric acid, acetic acid, formaldehyde and paraffin wax were from Carlo Erba (Milan, IT).
Peptide synthesis
Synthesis of the peptide gH625 (NH2-HGLASTLTRWAHYNALIRAF-CONH2) was performed via standard solid-phase-9-fluorenylmethoxycarbonyl (Fmoc) chemistry as previously reported29. The peptide was obtained with a yield of 30–40% and purity was higher than 98%. Labelling of the N-terminus with 4-chloro-7-nitrobenz-2-oxa-1,3-diazole (NBD-Cl) to obtain NBD-gH625 was performed in N,N-Dimethylformamide (DMF) with 2 equivalents of N,N-Diisopropylethylamine (DIPEA) as previously reported23.
Animals
In vivo studies were performed in male Wistar rats housed under a 12 hours light-dark cycle with free access to food and water. The animals were allocated in five groups, each consisting of three rats. Three animal groups received a single i.v. administration of NBD-gH625 at a concentration of 10 µg, 20 µg, and 40 µg/100 g bw, respectively. Control group received vehicle while another group received gH-625 (40 µg/100 g bw). Both NBD-gH625 and gH625 were dissolved in phosphate-buffered saline. After 3.5 hours from the i.v. administration, the animals were anesthetized with Zoletil® (40 mg/100 g) and euthanized by decapitation. This study was carried out in strict accordance with recommendations in the European Guide for the Care and Use of Laboratory Animals. Every effort was made to minimize animal pain and suffering. All animal protocols were approved by the Committee on the Ethics of Animal Experiments of the University of Napoli Federico II (Italy) and the Italian Minister of Health. (Protocol number 2012/000180).
Fluorescence microscopy analysis
The ex-vivo fluorescence microscopy analysis was performed to evaluate the distribution of NBD-gH625 on both sides of the BBB. In order to evaluate if there is a linear relationship between slides fluorescence integrated density and the amount of the peptide, a calibration curve was obtained. In particular, increasing amounts of NBD-gH625 (0–30 µM) were spotted on microscope slides and images at 515 nm were acquired (See the Results section) and analysed as described below. Brains were removed from animals, sectioned sagittally in thick slices, washed in PBS, mounted on coverslips, stained with DAPI (4′–6 Diamidino-2-Phenylindole, Dilactate) (Invitrogen, Carlsbad, CA, USA) and analysed under Axioskop fluorescence microscope (Zeiss). Images, at least 10 field of view (800 × 700 μm each) for each experimental class, were acquired using an AxioCam MRc5 (Zeiss) with DAPI filter (λex 350 nm; λem 461 nm) and a fluorescein isothiocyanate filter (λex 488 nm; λem 515 nm).
To evaluate the distribution of NBD-gH625 on both sides of the BBB, we estimated the fluorescence inside the blood vessels (without discriminating between the amount present in the blood and that present in the endothelial cells) and outside the blood vessels in 10 images for each experimental class. In detail, to assess the NBD-gH625 that reached without crossing the BBB, we selected blood vessels as the region of interest (ROI) (inbound) and evaluated the fluorescence intensity; then, on the non-zero thresholded images, an inversion of selected ROI was carried out to obtain the complementary ROI to calculate the amounts of NBD-gH625 which crossed the BBB (outbound).
The morphology of blood vessels was easily identified and outlined; the images were calibrated by ImageJ Rodbard function; integrated density values were calculated within the outlines exclusively, to be considered as inside fluorescence. Then, the thresholded and outlined images, to exclude both blood vessels and background values, were used to calculate the integrated density as outside fluorescence.
To evaluate the effect of concentration on the systemic delivery of NBD-gH625, a fluorescence microscopy analysis was performed as previously reported24.
Briefly, livers and brains were isolated and fixed for 24 hours in Bouin’s fixative (71% picric acid, 5% acetic acid, 24% formaldehyde) and embedded in paraffin wax (Carlo Erba, Milan, Italy). Tissue sections (10 μm of thickness) were incubated in 0.1% Sudan Black B dissolved in 70% ethanol for 20 minutes to reduce the tissues autofluorescence. The excess of Sudan Black B was removed by washing with Tris-buffered saline containing 0.02% Tween 2030,31. Sections were stained with DAPI to counterstain nuclei, then mounted with a coverslip in glycerol/phosphate-buffered saline (1:1) and acquired using an AxioCam MRc5 with DAPI filter (λex 350 nm; λem 461 nm) and a fluorescein isothiocyanate filter (λex 488 nm; λem 515 nm). All images were then analysed using Fiji 1.50 software to determine the mean fluorescence and the integrated density, defined as the product of the mean fluorescence per the region of interest (μm2)32. The percentage of delivered vs administered NBD-gH625 was calculated.
Statistical analysis
Statistical analysis was performed using GraphPad Prism 5.0. The two-tailed Mann Whitney t-test was used and P was considered significant if was at least less than 0.05.
Liposome preparation
Large unilamellar vesicles (LUVs) and small unilamellar vesicles (SUVs) consisting of PI/DOPE/DPPC/PS/Chol/SM (4/23/30/8/20/15 ratio in moles)33,34, DSPC/POPE/PI/PS/lysoPC/SM/DOPG (37/21/7/9/3/18/5 ratio in moles)35, and when required containing Rho-PE and NBD-PE, were formulated in 5 mM HEPES, 100 mM NaCl, pH 7.4. LUVs were prepared using the extrusion method as previously reported36; lipids were first dissolved in chloroform, then dried under a nitrogen gas stream and lyophilized overnight. For fluorescence experiments, buffer was added to dry lipid films and vortexed for 1 h; then the lipid suspension was freeze-thawed 6 times and extruded 20 times through polycarbonate membranes with 0.1 μm diameter pores to obtain LUVs. For circular dichroism measurements, peptide samples in SUVs were prepared using the following protocol37. Lipids were dissolved in chloroform and added to an equal volume of peptide solution dissolved in TFE containing appropriate peptide concentration. The samples were vortexed and lyophilized overnight. The dry samples were rehydrated with phosphate buffer (5 mM) for 1 h and sonicated for 30 min.
Membrane fluidity
LUVs containing Laurdan were prepared to determine membrane fluidity23. In order to insert Laurdan into the bilayer, it was added to lipid films before hydration. The peptide gH625 was added to LUVs at a P/L molar ratio of 0.5 and after 10 min the fluorescence spectra were recorded using a 1 cm path length quartz cell, thermostated at 25 °C or 37 °C. Spectra were corrected for the baseline signal. Laurdan emission spectra were recorded from 400 to 550 nm with λex 365 nm in the absence or presence of gH625 in 5 mM HEPES, 100 mM NaCl buffer (pH 7.4). Laurdan emission can shift from 440, in the ordered phase, to 490 in the disordered phase. The excitation generalized polarization (GP) was calculated as GP = (I440 − I490)/(I440 + I490) where I440 and I490 are the fluorescence intensities at the maximum emission wavelength in the ordered (λem 440 nm) and disordered (λem 490 nm) phases38.
Lipid mixing assays
Membrane lipid mixing was followed by the resonance energy transfer assay (FRET)39. The peptide was added to vesicles containing 0.6 mol % of two probes, NBD-PE (donor) and Rho-PE (acceptor), mixed with unlabelled vesicles at a 1:4 ratio (final lipid concentration 0.1 mM). The dilution of NBD-PE and Rho-PE due to membrane mixing produced an increase in NBD fluorescence (λex 465 nm, λem 530 nm) that was monitored at 37 °C as a function of added peptide. In order to avoid scattering interferences, a cut off filter (515 nm) between the sample and the emission monochromator was used. Complete mixing (100% level) was evaluated as the fluorescence intensity of vesicles after the addition of Triton X-100 (0.05% v/v) at the same total lipid concentrations of the fusion assay, while the zero level corresponded to the initial residual fluorescence of the vesicles. In order to get reproducible data and average results, lipid mixing experiments were repeated at least three times.
A modification of the lipid mixing experiment allowed to measure peptide-induced mixing of the inner monolayer40. A concentration of 0.6% mol for each of the fluorescent probes within the liposome was used. In order to completely reduce the NBD located at the outer surface of the membrane, LUVs were treated with sodium dithionite 100 mM (from a stock solution of 1 M dithionite in 1 M TRIS, pH 10.0) for approximately 1 h on ice in the dark. Excess sodium dithionite was removed by size exclusion chromatography through a Sephadex G-75 50 DNA Grade filtration column (GE Healthcare) eluted with a buffer containing 10 mM TRIS, 100 mM NaCl, and 1 mM EDTA, pH 7.4.
The ANTS/DPX experiment was used to evaluate leakage of encapsulated dyes induced by the peptide. The peptide in 5 mM Hepes and 100 mM NaCl at pH 7.4 was added to the stirred vesicle suspension (0.1 mM lipid) containing ANTS and DPX at 37 °C. Details of this assay have been previously reported41.
Tryptophan fluorescence measurements
Emission spectra of the tryptophan contained in the peptide (4 µM) in the absence or presence of target vesicles were recorded between 300 and 400 nm with λex 295 nm in order to determine the presence of the peptide inside the membrane. To establish the strength of peptide-lipid interaction, LUVs were added to the peptide solution (4 µM) and the fluorescence intensity was recorded as a function of the lipid/peptide molar ratio (L/P), in three to four separate experiments. The results were corrected for the dilution factor. We used an L/P ratio of 200:1. The obtained binding was described as a partition equilibrium: Xb = KpCf where Kp is the apparent partition coefficient in units of M−1, Xb is the molar ratio of bound peptide per total lipid and Cf is the equilibrium concentration of the free peptide in solution42. F∞ was obtained by extrapolation of a double reciprocal plot of the total peptide fluorescence vs the total lipid concentration in the outer leaflet. The fraction of membrane-bound peptide, fb, was determined by fb = (F − F0)/(F∞ − F0), where F represents the fluorescence of peptide after the addition of the vesicles and F0 represents the fluorescence of the unbound peptide. fb allowed us to calculate the equilibrium concentration of the free peptide in the solution, Cf, and the extent of peptide binding Xb. Values of Xb were corrected as Xb* = Xb/0.6, considering that the peptides were initially partitioned only over the outer leaflet of the SUV (60% the total lipid). The binding isotherm is the curve resulting from plotting Xb* versus the concentration of the free peptide, Cf.
Tryptophan quenching by acrylamide
A solution containing 4 µM of gH625 in the absence or presence of LUVs at a peptide/lipid molar ratio of 1/200, was titrated with the water-soluble quencher acrylamide (4 M mother solution). The maximal concentration of acrylamide in the samples is 0.2 M. Fluorescence was measured with λex 295 nm and λem 340 nm43. The data were analysed with the Stern-Volmer equation43, F0/F = 1 + Ksv [Q], where F0 and F represent the fluorescence intensities in the absence and the presence of the quencher (Q), respectively. The Ksv is the Stern-Volmer quenching constant, and is correlated to the accessibility of the tryptophan residue to acrylamide. As acrylamide does not significantly partition into the membrane bilayer, Ksv is a reliable reflection of the bimolecular rate constant for collisional quenching of the aromatic residues present in the aqueous phase43. Ksv is thus determined by the amount of non-lipid-associated free peptide as well as the peptide fraction located on the surface of the bilayer.
Circular dichroism spectroscopy
CD spectra were recorded at room temperature on a Jasco J-715 spectropolarimeter in a 0.1 cm quartz cell. The spectra are an average of 3 consecutive scans from 260 to 190 nm, recorded with a band width of 3 nm, a time constant of 16 s, and a scan rate of 10 nm/min. Spectra were recorded and corrected for the blank. Mean residue ellipticities (MRE) were calculated as MRE = Obsd/lcn (Obsd is the ellipticity measured in millidegrees, l is the path length of the cell in cm, c is the peptide concentration in mol/l, and n is the number of amino acid residues in the peptide). A solution of 8 µM of peptide with SUVs, was prepared as previously described37. The measurements were performed at P/L ratio of 0.08 mol/mol in SUVs consisting of PI/DOPE/DPPC/PS/Chol/SM (4/23/30/8/20/15 ratio in moles) and DSPC/POPE/PI/PS/lysoPC/SM/DOPG (37/21/7/9/3/18/5 ratio in moles). The percentage of helix was calculated from measurements of their mean residue ellipticity at 222 nm44. We used [ϑ]222 values of 0 and −40.000(1–2.5/n) deg cm2 dmol−1 per amino acid residue for 0% and 100% helicity; n is the number of amino acid residues. The ratio of the ellipticities at 222 and 208 nm were used to discriminate between monomeric and oligomeric states of helices45. The experiment was performed before and after centrifugation to remove eventual precipitated peptides from solution.
Results
Fluorescence microscopy analysis of rat tissues
To evaluate the amount of green fluorescence related to the peptide in brain, we compared the fluorescence of gH625 and NBD-gH625 treated tissue samples. To evaluate the suitability of this approach we used as internal control the DAPI fluorescence and found the same amount of fluorescence at 461 nm for both gH625 and NBD-gH625 (Supplementary Material S1). When we evaluated the fluorescence at 515 nm we found no emission for gH625, thus in our study samples from animals administered with gH625 were used as “blank”; conversely, we measured a consistent increase of fluorescence in NBD-gH625 samples (Fig. 1) being mostly of the cell-specific.
We thus used NBD-gH625 for all our analysis. The analysis of fluorescence values inside and outside blood brain vessels showed that NDB-gH625 reaches the BBB of treated animals (Fig. 2a) and/or crosses the BBB (Fig. 2b).
To evaluate the extent of this NBD-gH625 withdrawal from blood by liver sequestration, we compared different concentrations of NBD-gH625 injected in rats. Our data concerning fluorescence levels on brain slices, suggest that lower peptide concentrations are able to improve the reaching of the brain more compared to higher concentrations (Fig. 3a) as demonstrated by the highest concentration administered (40 μg) which produced an effect comparable to the control.
Fluorescence microscopy analysis of brain and liver slices of NBD-gH625 treatment. Experimental classes are expressed in μg per 100 gr of body weight. Scale bar 50 μm. (a) Integrated density of brain slices from rats injected with different concentration of NBD-gH625. **P < 0.01, ***P < 0.001. (b) Integrated density of liver slices from rats injected with different concentrations of NBD-gH625. **P < 0.01, ***P < 0.001. (c) Calibration curve representing the linear relationship between the known amounts of NBD-gH625 and the relative the integrated density obtained under the setup of the microscopy analysis system used. (d) Percentage of NBD-gH625 delivered in brain and liver after in vivo administration of NBD-gH625.
In the liver, we found that the lowest dose of NBD-gH625 has higher effect, giving rise to an increase of integrated density values compared to the higher ones, thus concentrating the fluorescence signal in narrow area (Fig. 3b); it remains to be determined whether this is due to a more effective removal of the peptide by Kupffer cells or a diffuse endothelial uptake as reported in literature46.
We also estimated the percentage of NBD-gH625 delivered in brain and liver, as the integrated density calibrated function of known amounts of NBD-gH625 (Fig. 3c). We showed that lower doses produced higher percentages of delivered peptide, while higher doses do not reach efficiently both organs (Fig. 3d).
Membrane fluidity
LUVs fluidity before and after the addition of gH625 were obtained using the fluorescent probe Laurdan47,48. Laurdan is able to insert into membranes and distribute equally between lipid phases; it has an emission maximum at 440 nm in gel phase membranes and at 490 nm in liquid phase membranes. The Generalized Polarization (GP) is a parameter commonly used to quantify the change in the lipid fluidity. LUVs composed of PI/DOPE/DPPC/PS/Chol/SM (4/23/30/8/20/15) mimicking the composition of the BBB34 and of DSPC/POPE/PI/PS/lysoPC/SM/DOPG (37/21/7/9/3/18/5) mimicking the composition of the liver35 were prepared. The lipid composition was chosen according to previous publications reporting the composition of membranes isolated from brain33,34 and liver35. The lipid composition of brain endothelial cells is unique, with an high amount of sphingomyelin (SM) and a lower content of phosphatidylcholine (PC) compared with other endothelial cells33. The relative abundance of Chol and SM, alters phospholipid packing within the membranes and phospholipid-cholesterol interactions. In particular, cholesterol interacts with sphingomylin forming rafts which influence phospholipid packing, membrane fluidity and obviously any translocation mechanism. The emission spectra of LUVs both mimicking the BBB and the liver clearly indicate the presence of ordered phases at 37 and at 25 °C; the reproducibility of the spectra after 24 h further supported that LUVs were stable and not leaky in the condition used for the experiments. The GP parameter allowed quantifying the effect of the peptide (Table 1). The fluidity of the membranes at 37 °C in the presence of gH625 was not modified significantly. In the case of BBB mimicking liposomes we observe a slight decrease of the GP parameter, indicating a shift towards more fluid membranes; on the contrary for liver mimicking liposomes we observe a slight increase of the GP value.
Ability of gH625 to induce lipid mixing
To investigate the fusogenicity of gH625 in LUVs mimicking the composition of the BBB and of the liver, we prepared LUVs composed of PI/DOPE/DPPC/PS/Chol/SM (4/23/30/8/20/15), for the BBB and of DSPC/POPE/PI/PS/lysoPC/SM/DOPG (37/21/7/9/3/18/5), for the liver.
Increasing amounts of gH625 were added to a population of LUVs labelled with NBD (donor) and Rho (acceptor) mixed with a population of unlabelled LUVs. Fusion determines a dequenching of the donor fluorescence as a result of dilution of fluorescent vesicles. The dependence of the extent of lipid mixing on the peptide to lipid molar ratio (P/L) was analyzed and reported in Fig. 4.
Interestingly, we observed a different behavior which depended on the lipid composition of LUVs. The graphs clearly show that gH625 has higher fusogenic ability in LUVs mimicking the composition of the BBB. At a peptide/lipid ratio 10 times lower compared to the liver (maximum P/L = 0.05 in BBB; maximum P/L = 0.7 in liver) we observe complete fusion of vesicles. It is likely that the cholesterol is involved in the higher fusogenic ability of gH625 in LUVs mimicking the BBB, as we previously reported15,49.
In the inner monolayer assay, the fluorescence from the vesicle membranes’ outer monolayer is eliminated by the addition of an aqueous reducing agent; while in the lipid mixing experiment we measured both hemi-fusion and complete fusion, in this experiment we determined only the extent of lipid mixing between the inner monolayers. Figure 4 reports the results obtained for liposomes mimicking the BBB and the liver and shows that while for LUVs mimicking the BBB we observe approximately 20% of inner monolayer fusion at a P/L ratio corresponding to 100% of fusion, for the liver LUVs we have 100% of inner monolayer fusion at a peptide/lipid ratio where we observe also 100% of lipid mixing. Thus, in liver mimicking liposomes we observe a complete fusion which includes also the inner monolayers and could be visualized as a complete denaturation of liposomes; this takes place at high P/L ratios. For the BBB mimicking liposomes, we observe high fusion ability at very low P/L ratios and very low inner monolayer fusion in this condition.
The ANTS/DPX assay is useful to determine eventual leakage of the liposomes; in both tested conditions gH625 did not present any leakage (data not shown).
We previously reported that this set of experiments can be considered as a qualitative indicator of translocation or bilayer perturbation bearing great significance for discriminating different mechanisms of interaction. We also support the view that vesicle fusion events non complemented by leakage of the aqueous contents of the vesicle may support promising applications for drug delivery; while fusion events also accompanied by leakage are typical of antimicrobial peptides (AMPs)15,50.
Tryptophan fluorescence emission analysis
The presence of a tryptophan residue in the middle of the sequence of gH625, allowed the evaluation of the degree of peptide penetration into liposomes of different composition. In particular, we compared the fluorescence emission spectra in vesicles mimicking the BBB and the liver with that in buffer. The quantum yield of aromatic residues of a peptide or protein normally changes when the amino acid is located in a more hydrophobic environment such as a phospholipid membrane, with an increase of the intensity of the fluorescence emission and a shift of the maximum toward shorter wavelengths (blue shift). Changes in the spectral properties were observed for both vesicles, suggesting that the single tryptophan residue of gH625 moves to a less polar environment upon interaction with lipids. Emission intensity was enhanced and a slight shift of the maxima towards lower wavelength was observed (Fig. 5). Blue shifts of this magnitude are typical of amphiphilic aromatic peptides interacting with membrane bilayers and are correlated to the aromatic moiety becoming partially immersed in the membrane. The observed blue shifts suggest that the peptide is capable of penetrating both lipid bilayers.
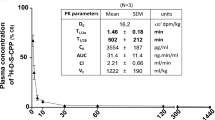
The change in fluorescence for the tryptophan binding to phospholipids was exploited to obtain binding isotherms for gH625 in the two different membrane mimetic environment and thus calculation of partition coefficients. The gH625 concentration is low enough to cause minimal aggregation in the aqueous phase and does not disrupt the bilayer structure. In order to determine the surface partition coefficients in LUVs mimicking the BBB and the liver, the fluorescence intensities were converted to moles of bound peptide per moles of lipid and plotted as a function of the free peptide concentration (Cf) as described in the experimental section. Partition coefficients depend on the concentration of lipid accessible to peptide, thus the curves obtained by plotting Xb* (the molar ratio of bound peptide per 60% of the total lipid) vs Cf (the equilibrium concentration of free peptide in the solution) are referred to as the conventional binding isotherms and are reported in Fig. 6. The shape of the binding isotherm was analyzed to get some insights into the organization of the peptide within the membrane; in fact, a straight line indicates a simple adhesion process, while a non-linear graph indicates a cooperative association of the peptide on the surface typical of peptides that self-associate at membrane surfaces upon partitioning. The shape of the isotherms obtained in both experimental conditions reflect a process whereby peptides first incorporate into the membrane and then aggregate there within; the opposite course of the isotherms would have been obtained in case of aggregation only in the water but not in the bilayer phase. The bound peptide (Xb*) slowly increases until a critical concentration is reached, where massive internal aggregation apparently starts to develop. The surface partition coefficients Kp were estimated by extrapolating the initial slopes of the curves to Cf values of zero. The Kp values are shown in Table 2. In particular, the Kp value obtained for the BBB is 5.7 104, indicating that the tryptophan in LUVs mimicking the BBB is able to interact significantly with the bilayer and that most of the peptide is located inside the liposomes; the Kp value for LUVs mimicking the liver is 5.7 103, indicating that also in this case the tryptophan is located inside the liposomes and is stably inserted but with a lower affinity.
Quenching of tryptophan by acrylamide
The observed changes in the tryptophan emission upon binding to lipid vesicles indicate gH625 insertion into the hydrophobic region of the bilayers. We determined the accessibility of the tryptophan residues of membrane bound peptides towards acrylamide, a neutral, water-soluble quencher, which is unable to penetrate into the hydrophobic core of the lipid bilayer. In fact, tryptophan residues more deeply buried inside the membrane are less strongly quenched. Stern-Volmer plots for the quenching of tryptophan by acrylamide are shown in Fig. 7.
In the presence of both types of LUVs, a great decrease in fluorescence intensity was evident, thus revealing that the tryptophan is less accessible to the quencher. In fact, the values for Ksv were lower (Table 2) in LUVs, suggesting that the tryptophan is more buried in the bilayers. Results clearly show that the tryptophan is well-inserted inside the bilayer in both situations but we observe a deeper insertion for the LUVs mimicking the BBB.
Secondary structure
Since the structural conformation has been shown to relate to internalization, the secondary structure was determined by CD spectroscopy as measured in water and in liposomes of the two different compositions to reveal changes of the secondary structure with respect to different experimental conditions (Fig. 8).
gH625 exhibits a mainly random coil structure in aqueous solution. In the presence of SUVs mimicking the BBB and the liver, the peptide assumes a helical conformation with two negative bands at about 208 and 222 nm. The calculations of helix content according to Chakrabartty et al.44 gives a 58% for gH625 in SUVs mimicking the BBB and 40% in SUVs mimicking the liver. Notwithstanding the percentages of helix calculated, the visual analysis of the spectra clearly indicates a more significant helical structure for BBB.
To determine whether we were also observing oligomerization processes in the experimental condition used for our assays we calculated the ratio of the ellipticities at 222 and 208 nm, which helps in discriminating between monomeric and oligomeric states of helices45. In fact, when the ratio θ222/θ208 is lower than 0.8, the peptide is essentially in its monomeric state, and when the ratio exceeds the value of 1.0, it is in its oligomeric state. The data reveal that in both conditions, gH625 adopts a α-helical conformation with the monomer/oligomer equilibrium shifted toward the monomeric state with a ratio θ222/θ208 of approximately 0.68 in SUVs mimicking the BBB and 0.45 in SUVs mimicking the liver. Moreover, as expected we did not observe any effect on the spectra after centrifugation to remove eventually precipitated peptides from solution.
The change of conformation from random to helical is a key feature and the driving force of peptides able to enter the bilayer. Thus, the obtained results clearly indicate that gH625 is able to change from a random coil to a helical structure in vesicles mimicking the BBB, while the conformational change is much less evident in vesicles mimicking the liver.
Discussion
We previously found that gH625 can facilitate brain delivery24 although the mechanism by which gH625 mediates the crossing of the BBB and liver barriers remains unclear. We focussed on the fact that probably the mechanisms promoting uptake is different. While much is known on how gH625 is crossing the membranes of eukaryotic cells in general less is known specifically for liver and BBB.
Our previous findings showed that gH625 was able to reach the brain after intravenous injection, despite macrophages of liver (Kupffer cells), seem to sequestrate the peptide from circulation24. We also previously reported that gH625 is worth for further development as a suitable device to enhance drug delivery beyond the BBB since it presents a high serum stability (after 3.5 h of incubation we could find still a significant amount of intact peptide) and the percentage of uptake in human neuroblastoma and glioblastoma astrocytoma is around 80–90%24. Nonetheless, we did not perform a comparative evaluation of the BBB uptake with that of the liver. Any such information is crucial for the eventual application of gH625.
Thus, this work enlarges our knowledge on the biodistribution of gH625 in an animal model showing that in vivo administration of gH625 permits to reach the BBB, although part of the peptide is sequestered by liver. In particular, our data clearly show that gH625 reaches the BBB and crosses it; this is the first in vivo quantification of gH625 crossing the BBB. Interestingly, we demonstrated that gH625 is able to reach the brain at lower doses injected with higher percentages of delivered peptide compared to the liver. These data further show that, despite the liver is able to withdraw gH625, and although we cannot state whether the reason of the liver accumulation is macrophage activation with consequent gH625 removal or endothelial generalized uptake, the administration of lower amounts of peptide should be more effective for brain delivery.
The comprehension of the mechanism of interaction of gH625 with model membranes mimicking the BBB and the liver allows obtaining key information, which could be useful for the design of novel drug delivery vectors. It is important to note that CPPs present numerous similarities with AMPs in charge, structure etc. and it is key to understand how these parameters can influence their interaction with the membrane and affect their translocation ability and cytotoxicity50,51. In particular, we observed that gH625 presents a greater fusion ability for membranes mimicking the BBB while lower fusion ability for liver mimicking membranes; moreover, from the inner monolayer experiment, we note that in condition where we observe complete lipid mixing we do not observe significant inner monolayer mixing while for liver membranes in condition with complete lipid mixing we have also significant inner monolayer mixing. This result clearly indicates that we have hemi-fusion only (outer membrane fusion) for BBB membranes and complete fusion for liver. The results obtained can also be correlated to the presence of a high percentage of cholesterol which is typical of lipid rafts. It is well known that BBB endothelial membranes are characterized by lipid rafts and we also previously reported the higher ability of gH625 to interact with membranes containing a high amount of cholesterol26,27,52. Moreover, we do not observe leakage in both conditions, which is key for eventual applications in drug delivery and discriminates CPPs from antimicrobial peptides53,54,55. Furthermore, these experiments hold great importance as qualitative indicators of translocation or bilayer perturbation bearing great significance for penetration across bilayers.
The analysis of the fluorescence spectra allowed the determination of affinity constants for the BBB and the liver membranes and further supports our results indicating a stronger interaction with the BBB and a deeper insertion of the tryptophan inside liposomes mimicking the BBB.
Secondary structure plays a major role in the uptake; thus, a key experiment is the determination of the conformation in different environments. A conformational change is key for modulation of peptide/lipid interactions and in particular, structural plasticity (the ability to change conformation according to the environment) has a crucial role in penetration across the membranes. In our study, we clearly observe a different structure of gH625 when moving from an aqueous solution to membranes. When in aqueous solution, the peptide has a random coil structure, but in the membranes it adopts a helical conformation with a higher helical content in membranes mimicking the BBB. Changes in the secondary structures are key for the translocation across membranes and the change in secondary structure represents the driving force for the penetration. This result is consistent with previous finding showing that pVEC adopts a β-sheet structure and TP10 becomes α-helical9,56,57.
Conclusions
One of the major challenges of current research is drug delivery for Central Nervous System (CNS) associated pathologies such as Alzheimer, Parkinson, brain injury, cancer58,59. Intravenous administration may represent a relatively non-invasive route of drug delivery; however, the BBB is a key obstacle for both small and large molecules58,60. Improvement of brain delivery and reduction of systemic exposure of drugs are key points which may enable delivery of therapeutics from the bloodstream to the brain61,62. To better understand and ameliorate the physicochemical properties of peptide drug delivery vectors to improve accumulation on target tissue, biodistribution studies are of great relevance. As a general rule, organs with high blood flow and rich in reticulo-endothelial system such as liver, could accumulate cell penetrating peptides63,64. Biodistribution analysis on other CPPs showed that the distribution among the different tissue depends on the peptide but all present a high liver distribution9,13.
Overall, our results indicate that the physicochemical properties such as the secondary structure in aqueous and membrane environments influence the cellular uptake mechanism and thus the biological properties (Fig. 9). In fact, despite the liver withdrawal of gH625, this peptide has the ability to reach and cross the BBB and this feature is ameliorated by lowering its concentration in blood. In conclusion, BBB peptide shuttles such as gH625 are a valid opportunity to enhance brain delivery of therapeutics and biophysical studies may be useful in improving their advantages compared to other drug delivery tools.
References
Kusuhara, H. & Sugiyama, Y. Efflux transport systems for drugs at the blood–brain barrier and blood–cerebrospinal fluid barrier (Part 1). Drug Discovery Today 6, 150–156, https://doi.org/10.1016/S1359-6446(00)01632-9 (2001).
Kusuhara, H. & Sugiyama, Y. Efflux transport systems for drugs at the blood–brain barrier and blood–cerebrospinal fluid barrier (Part 2). Drug Discovery Today 6, 206–212, https://doi.org/10.1016/S1359-6446(00)01643-3 (2001).
Mukherjee, B. Nanosize drug delivery system. Curr Pharm Biotechnol 14, 1221 (2013).
Zappavigna, S. et al. Nanocarriers Conjugated with Cell Penetrating Peptides: New Trojan Horses by Modern Ulysses. Curr Pharm Biotechnol 17, 700–722 (2016).
Kristensen, M. & Brodin, B. Routes for Drug Translocation Across the Blood-Brain Barrier: Exploiting Peptides as Delivery Vectors. Journal of Pharmaceutical Sciences 106, 2326–2334, https://doi.org/10.1016/j.xphs.2017.04.080 (2017).
Yang, H. Nanoparticle-mediated brain-specific drug delivery, imaging, and diagnosis. Pharm Res 27, 1759–1771, https://doi.org/10.1007/s11095-010-0141-7 (2010).
Hervé, F., Ghinea, N. & Scherrmann, J.-M. CNS Delivery Via Adsorptive Transcytosis. The AAPS Journal 10, 455–472, https://doi.org/10.1208/s12248-008-9055-2 (2008).
Zhang, D., Wang, J. & Xu, D. Cell-penetrating peptides as noninvasive transmembrane vectors for the development of novel multifunctional drug-delivery systems. J. Control. Release 229, 130–139, https://doi.org/10.1016/j.jconrel.2016.03.020 (2016).
Stalmans, S. et al. Cell-Penetrating Peptides Selectively Cross the Blood-Brain Barrier In Vivo. PLoS One 10, e0139652, https://doi.org/10.1371/journal.pone.0139652 (2015).
Zou, L. L., Ma, J. L., Wang, T., Yang, T. B. & Liu, C. B. Cell-penetrating Peptide-mediated therapeutic molecule delivery into the central nervous system. Curr Neuropharmacol 11, 197–208, https://doi.org/10.2174/1570159x11311020006 (2013).
Simon, M. J., Kang, W. H., Gao, S., Banta, S. & Iii, B. M. TAT Is Not Capable of Transcellular Delivery Across an Intact Endothelial Monolayer In Vitro. Annals of Biomedical Engineering 39, 394–401, https://doi.org/10.1007/s10439-010-0144-x (2011).
Li, S.-D. & Huang, L. Pharmacokinetics and Biodistribution of Nanoparticles. Molecular Pharmaceutics 5, 496–504, https://doi.org/10.1021/mp800049w (2008).
Sánchez-Navarro, M., Giralt, E. & Teixidó, M. Blood–brain barrier peptide shuttles. Current Opinion in Chemical Biology 38, 134–140, https://doi.org/10.1016/j.cbpa.2017.04.019 (2017).
Galdiero, S. et al. Intracellular delivery: exploiting viral membranotropic peptides. Curr Drug Metab 13, 93–104 (2012).
Galdiero, S., Falanga, A., Morelli, G. & Galdiero, M. gH625: a milestone in understanding the many roles of membranotropic peptides. Biochim Biophys Acta 1848, 16–25, https://doi.org/10.1016/j.bbamem.2014.10.006 (2015).
Guarnieri, D. et al. Shuttle-mediated nanoparticle delivery to the blood-brain barrier. Small 9, 853–862, https://doi.org/10.1002/smll.201201870 (2013).
Tarallo, R. et al. Clickable functionalization of liposomes with the gH625 peptide from Herpes simplex virus type I for intracellular drug delivery. Chemistry 17, 12659–12668, https://doi.org/10.1002/chem.201101425 (2011).
Borchmann, D. E. et al. Membranotropic peptide-functionalized poly(lactide)- graft -poly(ethylene glycol) brush copolymers for intracellular delivery. Macromolecules 48, 942–949, https://doi.org/10.1021/acs.macromol.5b00173 (2015).
Carberry, T. P. et al. Dendrimer functionalization with a membrane-interacting domain of herpes simplex virus type 1: towards intracellular delivery. Chemistry 18, 13678–13685, https://doi.org/10.1002/chem.201202358 (2012).
Falanga, A. et al. Elucidation of the interaction mechanism with liposomes of gH625-peptide functionalized dendrimers. PLoS One 9, e112128, https://doi.org/10.1371/journal.pone.0112128 (2014).
Tarallo, R. et al. Dendrimers functionalized with membrane-interacting peptides for viral inhibition. Int J Nanomedicine 8, 521–534, https://doi.org/10.2147/ijn.s37739 (2013).
Perillo, E. et al. Quantitative and qualitative effect of gH625 on the nanoliposome-mediated delivery of mitoxantrone anticancer drug to HeLa cells. Int J Pharm 488, 59–66, https://doi.org/10.1016/j.ijpharm.2015.04.039 (2015).
Falanga, A. et al. Dimerization in tailoring uptake efficacy of the HSV-1 derived membranotropic peptide gH625. Sci Rep 7, 9434, https://doi.org/10.1038/s41598-017-09001-x (2017).
Valiante, S. et al. Peptide gH625 enters into neuron and astrocyte cell lines and crosses the blood-brain barrier in rats. Int J Nanomedicine 10, 1885–1898, https://doi.org/10.2147/ijn.s77734 (2015).
Galdiero, S. et al. Structure and orientation of the gH625-644 membrane interacting region of herpes simplex virus type 1 in a membrane mimetic system. Biochemistry 51, 3121–3128, https://doi.org/10.1021/bi201589m (2012).
Galdiero, S. et al. The presence of a single N-terminal histidine residue enhances the fusogenic properties of a Membranotropic peptide derived from herpes simplex virus type 1 glycoprotein H. J Biol Chem 285, 17123–17136, https://doi.org/10.1074/jbc.M110.114819 (2010).
Galdiero, S. et al. Analysis of a membrane interacting region of herpes simplex virus type 1 glycoprotein H. J Biol Chem 283, 29993–30009, https://doi.org/10.1074/jbc.M803092200 (2008).
Vitiello, G. et al. Fusion of raft-like lipid bilayers operated by a membranotropic domain of the HSV-type I glycoprotein gH occurs through a cholesterol-dependent mechanism. Soft Matter 11, 3003–3016, https://doi.org/10.1039/c4sm02769h (2015).
Caporale, A., Doti, N., Sandomenico, A. & Ruvo, M. Evaluation of combined use of Oxyma and HATU in aggregating peptide sequences. J Pept Sci 23, 272–281, https://doi.org/10.1002/psc.2977 (2017).
Baschong, W., Suetterlin, R. & Laeng, R. H. Control of autofluorescence of archival formaldehyde-fixed, paraffin-embedded tissue in confocal laser scanning microscopy (CLSM). J Histochem Cytochem 49, 1565–1572 (2001).
Viegas, M. S., Martins, T. C., Seco, F. & do Carmo, A. An improved and cost-effective methodology for the reduction of autofluorescence in direct immunofluorescence studies on formalin-fixed paraffin-embedded tissues. Eur J Histochem 51, 59–66 (2007).
Vonesch, C. & Unser, M. A fast thresholded landweber algorithm for wavelet-regularized multidimensional deconvolution. IEEE Trans Image Process 17, 539–549, https://doi.org/10.1109/tip.2008.917103 (2008).
Siakotos, A. N., Rouser, G. & Fleischer, S. Isolation of highly purified human and bovine brain endothelial cells and nuclei and their phospholipid composition. Lipids 4, 234–239, https://doi.org/10.1007/bf02532638 (1969).
Campbell, S. D., Regina, K. J. & Kharasch, E. D. Significance of Lipid Composition in a Blood Brain Barrier-Mimetic PAMPA Assay. Journal of biomolecular screening 19, 437–444, https://doi.org/10.1177/1087057113497981 (2014).
Ray, T. K., Spski, V. P., Brclay, M., Essner, E. & Archibald, F. M. Lipid Composition of Rat Liver Plasma Membranes. J. Biol. Chem. 244, 5528–5536 (1969).
Hope, M. J., Bally, M. B., Webb, G. & Cullis, P. R. Production of large unilamellar vesicles by a rapid extrusion procedure: characterization of size distribution, trapped volume and ability to maintain a membrane potential. Biochim Biophys Acta 812, 55–65 (1985).
Han, X., Steinhauer, D. A., Wharton, S. A. & Tamm, L. K. Interaction of Mutant Influenza Virus Hemagglutinin Fusion Peptides with Lipid Bilayers: Probing the Role of Hydrophobic Residue Size in the Central Region of the Fusion Peptide. Biochemistry 38, 15052–15059, https://doi.org/10.1021/bi991232h (1999).
Amaro, M., Reina, F., Hof, M., Eggeling, C. & Sezgin, E. Laurdan and Di-4-ANEPPDHQ probe different properties of the membrane. Journal of Physics D: Applied Physics 50, 134004 (2017).
Struck, D. K., Hoekstra, D. & Pagano, R. E. Use of resonance energy transfer to monitor membrane fusion. Biochemistry 20, 4093–4099 (1981).
Cummings, J. E. & Vanderlick, T. K. Aggregation and hemi-fusion of anionic vesicles induced by the antimicrobial peptide cryptdin-4. Biochim Biophys Acta 1768, 1796–1804, https://doi.org/10.1016/j.bbamem.2007.04.016 (2007).
Parente, R. A., Nir, S. & Szoka, F. C. Jr. Mechanism of leakage of phospholipid vesicle contents induced by the peptide GALA. Biochemistry 29, 8720–8728 (1990).
Schwarz, G., Stankowski, S. & Rizzo, V. Thermodynamic analysis of incorporation and aggregation in a membrane: application to the pore-forming peptide alamethicin. Biochim Biophys Acta 861, 141–151 (1986).
Eftink, M. R. & Ghiron, C. A. Exposure of tryptophanyl residues in proteins. Quantitative determination by fluorescence quenching studies. Biochemistry 15, 672–680 (1976).
Chakrabartty, A., Kortemme, T. & Baldwin, R. L. Helix propensities of the amino acids measured in alanine-based peptides without helix-stabilizing side-chain interactions. Protein Science 3, 843–852, https://doi.org/10.1002/pro.5560030514 (1994).
Galdiero, S. et al. Peptides containing membrane-interacting motifs inhibit herpes simplex virus type 1 infectivity. Peptides 29, 1461–1471, https://doi.org/10.1016/j.peptides.2008.04.022 (2008).
Lopez, B. G., Tsai, M. S., Baratta, J. L., Longmuir, K. J. & Robertson, R. T. Characterization of Kupffer cells in livers of developing mice. Comparative Hepatology 10, 2–2, https://doi.org/10.1186/1476-5926-10-2 (2011).
Parasassi, T., Conti, F. & Gratton, E. Time-resolved fluorescence emission spectra of Laurdan in phospholipid vesicles by multifrequency phase and modulation fluorometry. Cell Mol Biol 32, 103–108 (1986).
Maniti, O., Alves, I., Trugnan, G. & Ayala-Sanmartin, J. Distinct Behaviour of the Homeodomain Derived Cell Penetrating Peptide Penetratin in Interaction with Different Phospholipids. PLoS One 5, e15819, https://doi.org/10.1371/journal.pone.0015819 (2010).
Wang, H. & Eckel, R. H. What are lipoproteins doing in the brain? Trends in Endocrinology & Metabolism 25, 8–14, https://doi.org/10.1016/j.tem.2013.10.003 (2014).
Galdiero, S. et al. Antimicrobial peptides as an opportunity against bacterial diseases. Current Medicinal Chemistry 22, 1665–1677, https://doi.org/10.2174/0929867322666150311145632 (2015).
Falanga, A. & Galdiero, S. In Amino Acids, Peptides and Proteins: Vol. 42, 190–227 (The Royal Society of Chemistry, 2018).
Galdiero, S. et al. Fusogenic domains in herpes simplex virus type 1 glycoprotein H. J Biol Chem 280, 28632–28643, https://doi.org/10.1074/jbc.M505196200 (2005).
Galdiero, S. et al. Exploitation of viral properties for intracellular delivery. J Pept Sci 20, 468–478, https://doi.org/10.1002/psc.2649 (2014).
Thorén, P. E. G., Persson, D., Lincoln, P. & Nordén, B. Membrane destabilizing properties of cell-penetrating peptides. Biophysical Chemistry 114, 169–179, https://doi.org/10.1016/j.bpc.2004.11.016 (2005).
Hovakeemian, S. G., Liu, R., Gellman, S. H. & Heerklotz, H. Correlating antimicrobial activity and model membrane leakage induced by nylon-3 polymers and detergents. Soft Matter 11, 6840–6851, https://doi.org/10.1039/c5sm01521a (2015).
Song, J. et al. Cellular uptake of transportan 10 and its analogs in live cells: Selectivity and structure–activity relationship studies. Peptides 32, 1934–1941, https://doi.org/10.1016/j.peptides.2011.07.018 (2011).
Eiríksdóttir, E., Konate, K., Langel, Ü., Divita, G. & Deshayes, S. Secondary structure of cell-penetrating peptides controls membrane interaction and insertion. Biochimica et Biophysica Acta (BBA) - Biomembranes 1798, 1119–1128, https://doi.org/10.1016/j.bbamem.2010.03.005 (2010).
Sun, C. et al. Noninvasive nanoparticle strategies for brain tumor targeting. Nanomedicine: Nanotechnology, Biology and Medicine 13, 2605–2621, https://doi.org/10.1016/j.nano.2017.07.009 (2017).
Sweeney, M. D., Sagare, A. P. & Zlokovic, B. V. Blood–brain barrier breakdown in Alzheimer disease and other neurodegenerative disorders. Nature Reviews Neurology, https://doi.org/10.1038/nrneurol.2017.188 (2018).
Bicker, J., Alves, G., Fortuna, A. & Falcão, A. Blood–brain barrier models and their relevance for a successful development of CNS drug delivery systems: A review. European Journal of Pharmaceutics and Biopharmaceutics 87, 409–432, https://doi.org/10.1016/j.ejpb.2014.03.012 (2014).
Kou, L. et al. Transporter-Guided Delivery of Nanoparticles to Improve Drug Permeation across Cellular Barriers and Drug Exposure to Selective Cell Types. Frontiers in Pharmacology 9, 27 (2018).
Liebner, S. et al. Functional morphology of the blood–brain barrier in health and disease. Acta Neuropathologica 135, 311–336, https://doi.org/10.1007/s00401-018-1815-1 (2018).
Tian, X.-H. et al. In vitro and in vivo studies on gelatin-siloxane nanoparticles conjugated with SynB peptide to increase drug delivery to the brain. International Journal of Nanomedicine 7, 1031–1041, https://doi.org/10.2147/ijn.s26541 (2012).
Crawford, L., Rosch, J. & Putnam, D. Concepts, technologies, and practices for drug delivery past the blood–brain barrier to the central nervous system. J. Control. Release 240, 251–266, https://doi.org/10.1016/j.jconrel.2015.12.041 (2016).
Author information
Authors and Affiliations
Contributions
S.G., S.V. and G.M. contributed to the discussion, design the experiments and writing of the manuscript. A.F., L.L., E.P. and S.G. contributed to the peptides synthesis, fluorescence assays and CD measurements. G.I., A.L. and S.V. contributed performing in vivo experiments and analysis. S.G. organized the information in the main text.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Falanga, A., Iachetta, G., Lombardi, L. et al. Enhanced uptake of gH625 by blood brain barrier compared to liver in vivo: characterization of the mechanism by an in vitro model and implications for delivery. Sci Rep 8, 13836 (2018). https://doi.org/10.1038/s41598-018-32095-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-32095-w
Keywords
This article is cited by
-
Improved prediction and characterization of blood-brain barrier penetrating peptides using estimated propensity scores of dipeptides
Journal of Computer-Aided Molecular Design (2022)
-
Eradication of Candida albicans persister cell biofilm by the membranotropic peptide gH625
Scientific Reports (2020)
-
Quantum dots functionalized with gH625 attenuate QDs oxidative stress and lethality in Caenorhabditis elegans: a model system
Ecotoxicology (2020)
-
gH625-liposomes as tool for pituitary adenylate cyclase-activating polypeptide brain delivery
Scientific Reports (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.