Abstract
Purpose
We describe the preparation of injectable polymeric paste (IPP) formulations for local and sustained release of drugs. Furthermore, we include the characterization and possible applications of such pastes. Particular attention is paid to characteristics relevant to the successful clinical formulation development, such as viscosity, injectability, degradation, drug release, sterilization, stability performance and pharmacokinetics.
Methods
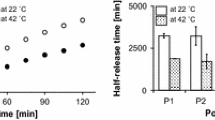
Paste injectability was characterized using measured viscosity and the Hagen-Poiseuille equation to determine injection forces. Drug degradation, release and formulation stability experiments were performed in vitro and drug levels were quantified using HPLC-UV methods. Pharmacokinetic evaluation of sustained-release lidocaine IPPs used five groups of six rats receiving increasing doses subcutaneously. An anti-cancer formulation was evaluated in a subcutaneous tumor xenograft mouse model.
Results
The viscosity and injectability of IPPs could be controlled by changing the polymeric composition. IPPs demonstrated good long-term stability and tunable drug-release with low systemic exposure in vivo in rats. Preliminary data in a subcutaneous tumor model points to a sustained anticancer effect.
Conclusions
These IPPs are tunable platforms for local and sustained delivery of drugs and have potential for further clinical development to treat a number of diseases.










Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the curve
- Cl:
-
Clearance
- Cmax :
-
Maximum observed concentration
- DMSO:
-
Dimethyl sulfoxide
- FDA:
-
Food and drug administration
- IPP:
-
Injectable polymeric paste
- LNCaP:
-
Androgen-sensitive human prostate adenocarcinoma cells
- mPEG:
-
Methoxy polyethylene glycol
- MRT:
-
Mean residence time
- NMP:
-
N-methyl-2-pyrrolidone
- PBS:
-
Phosphate buffered saline
- PCL:
-
Poly(caprolactone)
- PDLLA-MePEG:
-
Poly(DL-lactide)co-methoxyPEG)
- PEG:
-
Polyethylene glycol
- PGA:
-
Poly(glycolic acid)
- PLA:
-
Poly(lactic acid)
- PLGA:
-
Poly(lactic-co-glycolic acid)
- RP-HPLC-UV:
-
Reversed phase high-performance liquid chromatography with ultraviolet detection
- RT:
-
Retention time
- t1/2 :
-
Terminal half-life
- UPLC-MS/MS:
-
Ultra performance liquid chromatography - tandem mass spectrometry
- λz:
-
Terminal rate constant
References
Bregy A, Shah AH, Diaz MV, Pierce HE, Ames PL, Diaz D, et al. The role of Gliadel wafers in the treatment of high-grade gliomas. Expert Rev Anticancer Ther. 2013;13(12):1453–61.
Signore PE, Machan LS, Jackson JK, Burt H, Bromley P, Wilson JE, et al. Complete inhibition of intimal hyperplasia by perivascular delivery of paclitaxel in balloon-injured rat carotid arteries. J Vasc Interv Radiol. 2001;12(1):79–88.
Liggins RT, Cruz T, Min W, Liang L, Hunter WL, Burt HM. Intra-articular treatment of arthritis with microsphere formulations of paclitaxel: biocompatibility and efficacy determinations in rabbits. Inflamm Res. 2004;53(8):363–72.
Liggins RT, D'Amours S, Demetrick JS, Machan LS, Burt HM. Paclitaxel loaded poly(l-lactic acid) microspheres for the prevention of intraperitoneal carcinomatosis after a surgical repair and tumor cell spill. Biomaterials. 2000;21(19):1959–69.
Ernsting MJ, Hoang B, Lohse I, Undzys E, Cao P, Do T, et al. Targeting of metastasis-promoting tumor-associated fibroblasts and modulation of pancreatic tumor-associated stroma with a carboxymethylcellulose-docetaxel nanoparticle. J Control Release. 2015;206:122–30.
Liu Y, Wu Y, Lin H, Xiao Y, Zhu X, Zhang K, et al. Study on an injectable biomedical paste using cross-linked sodium hyaluronate as a carrier of hydroxyapatite particles. Carbohydr Polym. 2018;195:378–86.
Salehi G, Behnamghader A, Hesaraki S, Mozafari M. Synergistic effects of carbohydrate polymers on the performance of hybrid injectable bone pastes. Eur Polym J. 2019;119:523–30.
Ye H, Owh C, Jiang S, Ng CZQ, Wirawan D, Loh XJ. A Thixotropic Polyglycerol Sebacate-Based Supramolecular Hydrogel as an Injectable Drug Delivery Matrix. Polymers. 2016;8(4).
Boles L, Alexander C, Pace L, Haggard W, Bumgardner J, Jennings J. Development and Evaluation of an Injectable Chitosan/β-Glycerophosphate Paste as a Local Antibiotic Delivery System for Trauma Care. Journal of Functional Biomaterials. 2018;9(4).
Sivashanmugam A, Arun Kumar R, Vishnu Priya M, Nair SV, Jayakumar R. An overview of injectable polymeric hydrogels for tissue engineering. Eur Polym J. 2015;72:543–65.
Kondiah PJ, Choonara YE, Kondiah PP, Marimuthu T, Kumar P, Du Toit LC, et al. A review of injectable polymeric hydrogel systems for application in bone tissue engineering. Molecules. 2016;21(11):1580.
Cui X, Zhang Y, Wang H, Gu Y, Li L, Zhou J, et al. An injectable borate bioactive glass cement for bone repair: preparation, bioactivity and setting mechanism. J Non-Cryst Solids. 2016;432:150–7.
Zhang J, Liu W, Gauthier O, Sourice S, Pilet P, Rethore G, et al. A simple and effective approach to prepare injectable macroporous calcium phosphate cement for bone repair: syringe-foaming using a viscous hydrophilic polymeric solution. Acta Biomater. 2016;31:326–38.
De Pablo JJ, Qazvini NT, Sadati M, Tirrell M. Injectable pastes based on oppositely charged polymer/calcium phosphate nanoparticles. Google Patents; 2019.
Krasko MY, Golenser J, Nyska A, Nyska M, Brin YS, Domb AJ. Gentamicin extended release from an injectable polymeric implant. J Control Release. 2007;117(1):90–6.
Ickowicz DE, Abtew E, Khan W, Golovanevski L, Steinman N, Weiniger CF, et al. Poly (ester-anhydride) for controlled delivery of hydrophilic drugs. J Bioact Compat Polym. 2016;31(2):127–39.
Ahmed T. Review: approaches to develop PLGA based in situ gelling system with low initial burst. Pak J Pharm Sci. 2015;28(2):657–65.
Alexander A. Ajazuddin, Khan J, Saraf S, Saraf S. poly(ethylene glycol)-poly(lactic-co-glycolic acid) based thermosensitive injectable hydrogels for biomedical applications. J Control Release. 2013;172(3):715–29.
Chitkara D, Shikanov A, Kumar N, Domb AJ. Biodegradable injectable in situ depot-forming drug delivery systems. Macromol Biosci. 2006;6(12):977–90.
Ahmed TA, Ibrahim HM, Ibrahim F, Samy AM, Kaseem A, Nutan MT, et al. Development of biodegradable in situ implant and microparticle injectable formulations for sustained delivery of haloperidol. J Pharm Sci. 2012;101(10):3753–62.
Cho H, Gao J, Kwon GS. PEG-b-PLA micelles and PLGA-b-PEG-b-PLGA sol-gels for drug delivery. J Control Release. 2016;240:191–201.
El-Zaafarany GM, Soliman ME, Mansour S, Cespi M, Palmieri GF, Illum L, et al. A Tailored Thermosensitive PLGA-PEG-PLGA/Emulsomes Composite for Enhanced Oxcarbazepine Brain Delivery via the Nasal Route. Pharmaceutics. 2018;10(4).
Rahman CV, Kuhn G, White LJ, Kirby GT, Varghese OP, McLaren JS, et al. PLGA/PEG-hydrogel composite scaffolds with controllable mechanical properties. J Biomed Mater Res B Appl Biomater. 2013;101(4):648–55.
Rahman CV, Smith SJ, Morgan PS, Langmack KA, Clarke PA, Ritchie AA, et al. Adjuvant chemotherapy for brain tumors delivered via a novel intra-cavity moldable polymer matrix. PLoS One. 2013;8(10):e77435.
Zhao W, Li J, Jin K, Liu W, Qiu X, Li C. Fabrication of functional PLGA-based electrospun scaffolds and their applications in biomedical engineering. Mater Sci Eng C Mater Biol Appl. 2016;59:1181–94.
Wang L, Venkatraman S, Kleiner L. Drug release from injectable depots: two different in vitro mechanisms. J Control Release. 2004;99(2):207–16.
Winternitz CI, Jackson JK, Oktaba AM, Burt HM. Development of a polymeric surgical paste formulation for Taxol. Pharm Res. 1996;13(3):368–75.
Springate CM, Jackson JK, Gleave ME, Burt HM. Clusterin antisense complexed with chitosan for controlled intratumoral delivery. Int J Pharm. 2008;350(1–2):53–64.
Jackson JK, Zhang X, Llewellen S, Hunter WL, Burt HM. The characterization of novel polymeric paste formulations for intratumoral delivery. Int J Pharm. 2004;270(1–2):185–98.
Jackson JK, Min W, Cruz TF, Cindric S, Arsenault L, Von Hoff DD, et al. A polymer-based drug delivery system for the antineoplastic agent bis(maltolato)oxovanadium in mice. Br J Cancer. 1997;75:1014.
Jackson JK, Gleave ME, Yago V, Beraldi E, Hunter WL, Burt HM. The suppression of human prostate tumor growth in mice by the Intratumoral injection of a slow-release polymeric paste formulation of paclitaxel. Cancer Res. 2000;60(15):4146–51.
Zhang X, Jackson JK, Wong W, Min W, Cruz T, Hunter WL, et al. Development of biodegradable polymeric paste formulations for taxol: an in vitro and in vivo study. Int J Pharm. 1996;137(2):199–208.
Hoburg A, Keshlaf S, Schmidt T, Smith M, Gohs U, Perka C, et al. High-dose electron beam sterilization of soft-tissue grafts maintains significantly improved biomechanical properties compared to standard gamma treatment. Cell Tissue Bank. 2015;16(2):219–26.
Harrell CR, Djonov V, Fellabaum C, Volarevic V. Risks of using sterilization by gamma radiation: the other side of the coin. Int J Med Sci. 2018;15(3):274–9.
Sato N, Gleave ME, Bruchovsky N, Rennie PS, Goldenberg SL, Lange PH, et al. Intermittent androgen suppression delays progression to androgen-independent regulation of prostate-specific antigen gene in the LNCaP prostate tumour model. J Steroid Biochem Mol Biol. 1996;58(2):139–46.
Gleave M, Tolcher A, Miyake H, Nelson C, Brown B, Beraldi E, et al. Progression to androgen Independence is delayed by adjuvant treatment with antisense Bcl-2 Oligodeoxynucleotides after castration in the LNCaP prostate tumor model. Clin Cancer Res. 1999;5(10):2891.
Janik P, Briand P, Hartmann NR, Hansen M. The effect of Estrone-progesterone treatment on cell proliferation kinetics of hormone-dependent GR mouse mammary tumors. Cancer Res. 1975;35(12):3698.
Horoszewicz JS, Leong SS, Kawinski E, Karr JP, Rosenthal H, Chu TM, et al. LNCaP model of human prostatic carcinoma. Cancer Res. 1983;43(4):1809.
Rungseevijitprapa W, Bodmeier R. Injectability of biodegradable in situ forming microparticle systems (ISM). Eur J Pharm Sci. 2009;36(4):524–31.
Allmendinger A, Mueller R, Schwarb E, Chipperfield M, Huwyler J, Mahler H-C, et al. Measuring tissue Back-pressure - in vivo injection forces during subcutaneous injection. Pharm Res. 2015;32(7):2229–40.
Kapoor DN, Bhatia A, Kaur R, Sharma R, Kaur G, Dhawan S. PLGA: a unique polymer for drug delivery. Ther Deliv. 2015;6(1):41–58.
Bouissou C, Rouse JJ, Price R, van der Walle CF. The influence of surfactant on PLGA microsphere glass transition and water sorption: remodeling the surface morphology to attenuate the burst release. Pharm Res. 2006;23(6):1295–305.
Jain RA. The manufacturing techniques of various drug loaded biodegradable poly(lactide-co-glycolide) (PLGA) devices. Biomaterials. 2000;21(23):2475–90.
Siegel SJ, Kahn JB, Metzger K, Winey KI, Werner K, Dan N. Effect of drug type on the degradation rate of PLGA matrices. Eur J Pharm Biopharm. 2006;64(3):287–93.
Makadia HK, Siegel SJ. Poly lactic-co-glycolic acid (PLGA) as biodegradable controlled drug delivery carrier. Polymers. 2011;3(3):1377–97.
Athanasiou KA, Niederauer GG, Agrawal CM. Sterilization, toxicity, biocompatibility and clinical applications of polylactic acid/ polyglycolic acid copolymers. Biomaterials. 1996;17(2):93–102.
Baumann A, Tuerck D, Prabhu S, Dickmann L, Sims J. Pharmacokinetics, metabolism and distribution of PEGs and PEGylated proteins: quo vadis? Drug Discov Today. 2014;19(10):1623–31.
Parton T, King L, Parker G, Nesbitt A. The PEG moiety of Certolizumab Pegol is rapidly cleared from the blood of humans by the kidneys once it is cleaved from the Fab': P-0167. Inflamm Bowel Dis. 2009;15:S56.
Cairns M-L, Dickson GR, Orr JF, Farrar D, Hawkins K, Buchanan FJ. Electron-beam treatment of poly(lactic acid) to control degradation profiles. Polym Degrad Stab. 2011;96(1):76–83.
Loo JSC, Ooi CP, Boey FYC. Degradation of poly(lactide-co-glycolide) (PLGA) and poly(l-lactide) (PLLA) by electron beam radiation. Biomaterials. 2005;26(12):1359–67.
Drug monograph - lidocaine (systemic) [Internet]. [cited 08/08/2019]. Available from: https://accessmedicine.mhmedical.com/drugs.aspx#monoNumber=427085§ionID=223734024&tab=tab0.
Catterall WA, Mackie K. Local anesthetics. In: Brunton LL, Chabner BA, Knollmann BC, editors. Goodman & Gilman's: the pharmacological basis of therapeutics, 12e. New York: McGraw-Hill Education; 2011.
Benowitz NL. Chapter 9. Anesthetics, local. In: Olson KR, editor. Poisoning & drug overdose, 6e. New York: The McGraw-Hill Companies; 2012.
Levine L. Chronic orchialgia: evaluation and discussion of treatment options. Ther Adv Urol. 2010;2(5–6):209–14.
WebMD: Medscape Drugs & Diseases [Internet]. 2017 [cited 03/05/2016]. Available from: http://reference.medscape.com/drug/xylocaine-zingo-lidocaine-anesthetic-343363.
Eipe N, Gupta S, Penning J. Intravenous lidocaine for acute pain: an evidence-based clinical update. BJA Educ. 2016;16(9):292–8.
James ND, Sydes MR, Clarke NW, Mason MD, Dearnaley DP, Spears MR, et al. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet. 2016;387(10024):1163–77.
Sweeney CJCY, Carducci M, Liu G, Jarrard DF, Eisenberger M, Wong YN, et al. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. Urol Oncol. 2017;35(3):123.
Acknowledgements & Disclosures
We would like to thank Hans Adomat for performing the UHPLC/MS analysis for the rat PK study. We would like to state that the University of British Columbia has submitted a patent application on the injectable polymer paste formulation, listing Martin Gleave, John K. Jackson, Veronika Schmitt and Claudia Kesch as co-inventors. The technology has been outlicensed to Sustained Therapeutics, an early-stage biotech company founded by Dr. Gleave.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schmitt, V., Kesch, C., Jackson, J.K. et al. Design and Characterization of Injectable Poly(Lactic-Co-Glycolic Acid) Pastes for Sustained and Local Drug Release. Pharm Res 37, 36 (2020). https://doi.org/10.1007/s11095-019-2730-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-019-2730-4