Abstract
Purpose
To evaluate the function of multidrug and toxin extrusion proteins (MATEs) using 11C-labeled metformin ([11C]metformin) by positron emission tomography (PET).
Methods
PET was performed by intravenous bolus injection of [11C]metformin. Pyrimethamine at 0.5 and 5 mg/kg was intravenously administered to mice 30 min prior to the scan. Integration plot analysis was conducted for calculating liver (CLuptake,liver), kidney (CLuptake,kidney) tissue uptake, intrinsic biliary (CLint,bile) and urinary (CLint,urine) excretion clearances of [11C]metformin.
Results
Visualization by PET showed that pyrimethamine increased concentrations of [11C]metformin in the liver and kidneys, and decreased the concentrations in the urinary bladder without changing the blood profiles. Pyrimethamine had no effect on the CLuptake,liver and CLuptake,kidney, which were similar to the blood-flow rate. CLint,bile with regard to the liver concentration was unable to be determined, but administration of 0.5 and 5 mg/kg of pyrimethamine increased the liver-to-blood ratio to 1.6 and 2.3-fold, respectively, indicating that pyrimethamine inhibited the efflux of [11C]metformin from the liver. CLint,urine with regard to the corticomedullary region concentrations was decreased 37 and 68% of the control by administration of 0.5 and 5 mg/kg of pyrimethamine, respectively (P < 0.05).
Conclusions
Tissue concentration based investigations using [11C]metformin by PET enables the functional analysis of MATEs in the liver and kidneys.






Similar content being viewed by others
Abbreviations
- AUC:
-
The area under the concentration-time curve
- CLint,bile or urine :
-
The intrinsic bile or urinary excretion clearances
- CLrenal :
-
The renal clearance
- CLtot :
-
The total body clearance
- CLuptake,organ :
-
The uptake clearance in the liver or kidney
- MATEs:
-
Human multidrug and toxin extrusion proteins
- mMates:
-
Mouse multidrug and toxin extrusion proteins
- OCTs:
-
Human organic cation transporters
- mOcts:
-
Mouse organic cation transporters
- PET:
-
Positron emission tomography
- ROIs:
-
Regions of interest
- VE :
-
Extravascular space volume
- VOIs:
-
Volumetric regions of interest
References
Wang DS, Jonker JW, Kato Y, Kusuhara H, Schinkel AH, Sugiyama Y. Involvement of organic cation transporter 1 in hepatic and intestinal distribution of metformin. J Pharmacol Exp Ther. 2002;302:510–5.
Ito S, Kusuhara H, Kuroiwa Y, Wu C, Moriyama Y, Inoue K, et al. Potent and specific inhibition of mMate1-mediated efflux of type I organic cations in the liver and kidney by pyrimethamine. J Pharmacol Exp Ther. 2010;333:341–50.
Kusuhara H, Ito S, Kumagai Y, Jiang M, Shiroshita T, Moriyama Y, et al. Effects of a MATE protein inhibitor, pyrimethamine, on the renal elimination of metformin at oral microdose and at therapeutic dose in healthy subjects. Clin Pharmacol Ther. 2011;89:837–44.
Wang ZJ, Yin OQ, Tomlinson B, Chow MS. OCT2 polymorphisms and in-vivo renal functional consequence: studies with metformin and cimetidine. Pharmacogenet Genomics. 2008;18:637–45.
Shu Y, Brown C, Castro RA, Shi RJ, Lin ET, Owen RP, et al. Effect of genetic variation in the organic cation transporter 1, OCT1, on metformin pharmacokinetics. Clin Pharmacol Ther. 2008;83:273–80.
Umehara KI, Iwatsubo T, Noguchi K, Kamimura H. Functional involvement of organic cation transporter1 (OCT1/Oct1) in the hepatic uptake of organic cations in humans and rats. Xenobiotica. 2007;37:818–31.
Hillgren KM, Keppler D, Zur AA, Giacomini KM, Stieger B, Cass CE, et al. Emerging transporters of clinical importance: an update from the International Transporter Consortium. Clin Pharmacol Ther. 2013;94:52–63.
Yonezawa A, Inui K. Importance of the multidrug and toxin extrusion MATE/SLC47A family to pharmacokinetics, pharmacodynamics/toxicodynamics and pharmacogenomics. Br J Pharmacol. 2011;164:1817–25.
Otsuka M, Matsumoto T, Morimoto R, Arioka S, Omote H, Moriyama Y. A human transporter protein that mediates the final excretion step for toxic organic cations. Proc Natl Acad Sci U S A. 2005;102:17923–8.
Masuda S, Terada T, Yonezawa A, Tanihara Y, Kishimoto K, Katsura T, et al. Identification and functional characterization of a new human kidney-specific H+/organic cation antiporter, kidney-specific multidrug and toxin extrusion 2. J Am Soc Nephrol. 2006;17:2127–35.
Moriyama Y, Hiasa M, Matsumoto T, Omote H. Multidrug and toxic compound extrusion (MATE)-type proteins as anchor transporters for the excretion of metabolic waste products and xenobiotics. Xenobiotica. 2008;38:1107–18.
Terada T, Inui K. Physiological and pharmacokinetic roles of H+/organic cation antiporters (MATE/SLC47A). Biochem Pharmacol. 2008;75:1689–96.
Tanihara Y, Masuda S, Sato T, Katsura T, Ogawa O, Inui K. Substrate specificity of MATE1 and MATE2-K, human multidrug and toxin extrusions/H(+)-organic cation antiporters. Biochem Pharmacol. 2007;74:359–71.
Christensen MM, Pedersen RS, Stage TB, Brasch-Andersen C, Nielsen F, Damkier P, et al. A gene-gene interaction between polymorphisms in the OCT2 and MATE1 genes influences the renal clearance of metformin. Pharmacogenet Genomics. 2013;23(10):526–34.
Becker ML, Visser LE, van Schaik RH, Hofman A, Uitterlinden AG, Stricker BH. Genetic variation in the multidrug and toxin extrusion 1 transporter protein influences the glucose-lowering effect of metformin in patients with diabetes: a preliminary study. Diabetes. 2009;58:745–9.
Stocker SL, Morrissey KM, Yee SW, Castro RA, Xu L, Dahlin A, et al. The effect of novel promoter variants in MATE1 and MATE2 on the pharmacokinetics and pharmacodynamics of metformin. Clin Pharmacol Ther. 2013;93(2):186–94.
Tsuda M, Terada T, Ueba M, Sato T, Masuda S, Katsura T, et al. Involvement of human multidrug and toxin extrusion 1 in the drug interaction between cimetidine and metformin in renal epithelial cells. J Pharmacol Exp Ther. 2009;329(1):185–91.
Grun B, Kiessling MK, Burhenne J, Riedel KD, Weiss J, Rauch G, et al. Trimethoprim-metformin interaction and its genetic modulation by OCT2 and MATE1 transporters. Br J Clin Pharmacol. 2013;76(5):787–96.
Watanabe T, Kusuhara H, Sugiyama Y. Application of physiologically based pharmacokinetic modeling and clearance concept to drugs showing transporter-mediated distribution and clearance in humans. J Pharmacokinet Pharmacodyn. 2010;37:575–90.
Kusuhara H. Imaging in the study of membrane transporters. Clin Pharmacol Ther. 2013;94:33–6.
Ijuin R, Takashima T, Watanabe Y, Sugiyama Y, Suzuki M. Synthesis of [11C]dehydropravastatin, a PET probe potentially useful for studying OATP1B1 and MRP2 transporters in the liver. Bioorg Med Chem. 2012;20:3703–9.
Shingaki T, Takashima T, Ijuin R, Zhang X, Onoue T, Katayama Y, et al. Evaluation of oatp and Mrp2 activities in hepatobiliary excretion using newly developed positron emission tomography (PET) tracer, [11C]dehydropravastatin, in rats. J Pharmacol Exp Ther. 2013;347:193–202.
Takashima T, Nagata H, Nakae T, Cui Y, Wada Y, Kitamura S, et al. Positron emission tomography studies using (15R)-16-m-[11C]tolyl-17,18,19,20-tetranorisocarbacyclin methyl ester for the evaluation of hepatobiliary transport. J Pharmacol Exp Ther. 2010;335:314–23.
Takashima T, Kitamura S, Wada Y, Tanaka M, Shigihara Y, Ishii H, et al. PET imaging-based evaluation of hepatobiliary transport in humans with (15R)-11C-TIC-Me. J Nucl Med. 2012;53:741–8.
Takashima T, Hashizume Y, Katayama Y, Murai M, Wada Y, Maeda K, et al. The involvement of organic anion transporting polypeptide in the hepatic uptake of telmisartan in rats: PET studies with [11C]telmisartan. Mol Pharm. 2011;8:1789–98.
Takashima T, Wu C, Takashima-Hirano M, Katayama Y, Wada Y, Suzuki M, et al. Evaluation of breast cancer resistance protein function in hepatobiliary and renal excretion using PET with 11C-SC-62807. J Nucl Med. 2013;54:267–76.
Takashima T, Yokoyama C, Mizuma H, Yamanaka H, Wada Y, Onoe K, et al. Developmental changes in P-glycoprotein function in the blood–brain barrier of nonhuman primates: PET study with R-11C-verapamil and 11C-oseltamivir. J Nucl Med. 2011;52:950–7.
Hume WE, Shingaki T, Takashima T, Watanabe Y. The synthesis and biodistribution of [11C]metformin as a PET probe to study hepatobiliary transport mediated by the multi-drug and toxin extrusion transporter 1 (MATE1) in vivo. Bioorg Med Chem. 2013;21:7584–90.
Davies B, Morris T. Physiological parameters in laboratory animals and humans. Pharm Res. 1993;10:1093–5.
Tsuda M, Terada T, Mizuno T, Katsura T, Shimakura J, Inui K. Targeted disruption of the multidrug and toxin extrusion 1 (mate1) gene in mice reduces renal secretion of metformin. Mol Pharmacol. 2009;75:1280–6.
Zamek-Gliszczynski MJ, Hoffmaster KA, Tweedie DJ, Giacomini KM, Hillgren KM. Highlights from the international transporter consortium second workshop. Clin Pharmacol Ther. 2012;92(5):553–6.
Nakamura T, Yonezawa A, Hashimoto S, Katsura T, Inui K. Disruption of multidrug and toxin extrusion MATE1 potentiates cisplatin-induced nephrotoxicity. Biochem Pharmacol. 2010;80:1762–7.
Ito S, Kusuhara H, Yokochi M, Toyoshima J, Inoue K, Yuasa H, et al. Competitive inhibition of the luminal efflux by multidrug and toxin extrusions, but not basolateral uptake by organic cation transporter 2, is the likely mechanism underlying the pharmacokinetic drug-drug interactions caused by cimetidine in the kidney. J Pharmacol Exp Ther. 2012;340:393–403.
Somogyi A, Stockley C, Keal J, Rolan P, Bochner F. Reduction of metformin renal tubular secretion by cimetidine in man. Br J Clin Pharmacol. 1987;23:545–51.
Acknowledgments
We thank Mr. Masahiro Kurahashi of Sumitomo Heavy Industry Accelerator Service Ltd. for operation of the cyclotron. This study was partly carried out as the Research Project for the “Establishment of Evolutional Drug Development with the Use of Microdose Clinical Trial” sponsored by the New Energy and Industrial Technology Development Organization. Part of this work was also supported by JSPS KAKENHI Grant number 24229002.
Conflict of Interest
The authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
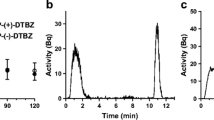
Supplemental Fig. 1
Time-radioactivity curves in the right ventricle obtained from PET imaging data analysis and the radioactivity in blood sample determined by gamma-counter. Open symbols represent control mice (n = 3; circles) and mice treated with 0.5 and 5 mg/kg of pyrimethamine (n = 4; triangles, n = 3; squares) from PET imaging data analysis. Closed symbols represent control mice (n = 3; circles) and mice treated with 0.5 and 5 mg/kg of pyrimethamine (n = 3; triangles, n = 3; squares) from blood sample determined by gamma-counter. (TIFF 68 kb)
Rights and permissions
About this article
Cite this article
Shingaki, T., Hume, W.E., Takashima, T. et al. Quantitative Evaluation of mMate1 Function Based on Minimally Invasive Measurement of Tissue Concentration Using PET with [11C]Metformin in Mouse. Pharm Res 32, 2538–2547 (2015). https://doi.org/10.1007/s11095-015-1642-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-015-1642-1