Abstract
Erythrocyte glutathione transferase (e-GST) is a detoxifying enzyme hyper-expressed in nephropathic patients and used recently as a biomarker for blood toxicity. Systemic sclerosis (SSc) is characterized by endothelial dysfunction and fibrosis of the skin and internal organs. Renal involvement is frequent in SSc patients. Here we show that e-GST is hyper-expressed in SSc patients (n=102) and correlates (R2=0.49, P<0.0001) with the Medsger DSS and DAI Valentini indices that quantify the severity and activity of this disease. Interestingly, e-GST does not correlate with the impairment of kidney or other specific organs taken separately. e-GST hyper-expression seems to be linked to the presence of a factor (i.e., toxin) that triggers the autoimmune disease, and not to the damage of specific organs or to oxidative stress. e-GST may be proposed as an innovative non-antibody biomarker for SSc useful to check the progress of this disease and the efficiency of new therapeutic strategies.
Similar content being viewed by others
Main
Systemic sclerosis (SSc) is an autoimmune disease that affects about 7 million people in the world causing hardening of connective tissue. It is characterized by vascular alterations, immune system activation and fibrosis of skin and internal organs.1 There are two major forms: limited cutaneous SSc (lcSSc) and diffuse cutaneous SSc (dcSSc). lcSSc involves cutaneous manifestations mainly affecting hands, arms and face.1 dcSSc affects a large area of the skin and one or more internal organs, frequently the kidneys, lungs, gastrointestinal tract and heart.1 There are no treatments for scleroderma itself, but individual organ system complications are treated.2, 3
The pathogenesis of SSc is complex and, although progress in the understanding of the multiple processes underlying SSc has been made in recent years, no single unifying hypothesis explaining all aspects of this disease exists.4 Over the years, it has been suggested that environmental as well as genetic risk factors predispose individuals to the onset of SSc. Environmental factors are likely to have a role in triggering disease because genetics does not provide a full justification for the development of SSc. However, reports on predisposing environmental factors are ambiguous, and meta-analyses are severely hindered by differences in the methodologies used for exposure measurement by individual studies, which unfortunately leaves a convincing environmental risk factor to be discovered.4 Immune activation is an early event in SSc. However, it is not known whether it is the initiating event or whether it is secondary endothelial damage. Endothelial cell injury might be triggered by vasculotropic viruses, inflammatory cytokines, granzymes, endothelial cell-specific autoantibodies or elevated levels of reactive oxygen species (ROS) due to oxidative stress. Endothelial damage and immune system activation lead to progressive skin and internal organs fibrosis.4
In this complicated context, the erythrocyte glutathione transferase (e-GST) is an attractive candidate to monitor the activity and severity and also to provide information about etiology of this disease. Glutathione transferases are a superfamily of detoxifying enzymes expressed in all human organs and devoted to the cell protection against endogenous or exogenous toxins.5 This role is achieved acting like catalysts of the conjugation of glutathione to toxic reactive compounds, thus promoting their inactivation and elimination. Alternatively, GSTs act as ligandins by binding many toxic nonreactive compounds and causing their elimination from the cell.5 These enzymes, and in particular e-GST, are hyper-expressed when the level of circulating toxins in the body increases, and we recently observed that higher concentrations of e-GST are present in subjects living in polluted areas.6 Similarly, nephropathic patients display elevated e-GST levels that correlate with the gravity of the kidney disease,7 and also this property is likely caused by abnormal levels of circulating toxins not filtered efficiently by the kidney. All these findings suggest that e-GST behaves like an endogenous biosensor, which reveals the levels of circulating toxic compounds and the efficiency of dialytic procedures.8 The rationale of the present study was that SSc often causes kidney damage and therefore a possible correlation might exist between the severity of this disease and e-GST expression. Renal disease remains one of the most important cause of morbidity and mortality in SSc,9 even if lung failure (both pulmonary hypertension and pulmonary fibrosis) seems to be the primary cause of scleroderma-related death today.10 The spectrum of renal complications in SSc includes scleroderma renal crisis, normotensive renal crisis, antineutrophil cytoplasmic antibodies-associated glomerulonephritis, penacillamine-associated renal disease, and reduced renal functional reserves manifested by proteinuria, microalbuminuria, or reduction in glomerular filtration rate.11 Moreover, given that a relevant oxidative stress is present in SSc patients,4 an increased e-GST activity is also possible.
The aim of the present study was to verify if e-GST activity is correlated to the severity or activity of this disease as evaluated using the Medsger Disease Severity Scale (DSS) and the Valentini Scleroderma Disease Activity Index (DAI).
Results
e-GST activity in sclerodermic patients correlates with DSS
As shown in Figure 1a and Table 1, the e-GST activity found in the overall population of SSc patients displays significant positive correlation with the DSS (R2=0.49, P<0.0001). A very similar positive correlation was also found, analyzing separately patients affected by the dcSSc as well as those affected by the lcSSc (Figures 1b and c and Table 1).
Correlation of e-GST with DSS and DAI. Correlation between e-GST and DSS. (a) All SSc patients (R2=0.49, P<0.0001). (b) Patients with lcSSc (R2=0.44, P<0.0001). (c) Patients with dcSSc (R2=0.54, P<0.0001). Correlation between e-GST and DAI. (d) All SSc patients (R2=0.49, P<0.0001). (e) Patients with lcSSc (R2=0.49, P<0.0001). (f) Patients with dcSSc (R2=0.48, P<0.0001). See also Table 1
e-GST activity in sclerodermic patients correlates positively with DAI
Also in the case of the DAI, which gives a quantitative estimation of the degree of activity of this disease, we found a positive correlation with the expression of e-GST both considering all sclerodermic patients (Figure 1d and Table 1; R2=0.49, P<0.0001) and when analyzing separately patients affected by the limited cutaneous or diffuse cutaneous scleroderma (Figures 1e and f and Table 1).
Catalase does not correlate with activity or severity of scleroderma
Catalase is one of the most potent scavengers of hydrogen peroxide and it is often proposed as a biomarker able to reveal oxidative stress in specific organs. In SSc patients, we observed an activity value of erythrocyte catalase (e-CAT), which is independent of the severity, both in patients affected by limited or diffuse SSc. e-CAT is also almost identical to that found in healthy subjects (Table 1). This result likely indicates that e-CAT expression is not linked to the e-GST expression and that the latter enzyme is not correlated to oxidative stress. This was also confirmed by the absence of correlation between e-GST and the endothelial dysfunction studied by flow-mediated dilation (FMD) (R2=0.074, P=0.045), a different index of oxidative stress.
Further strong evidence that e-GST activity parallels the severity of the disease is given in Figures 2a and b, where all SSc patients (or lcSSc and dcSSc patients) were grouped arbitrarily into three levels of severity (Table 2), on the basis of DSS, i.e., mild (1–5), moderate (6–9) and severe (>10). On the other hand, e-CAT is almost stable in all these patients (Figure 2 and Table 2). An identical behavior has been found by grouping arbitrarily the patients on the base of the degree of the activity of SSc, as evaluated by the DAI, i.e., mild (0.5–3), moderate (3.5–6) and severe (6.5–9) (Figures 2c and d and Table 2). The incremental factor observed for the average e-GST in the highest levels of severity and activity is given in Figure 2e and is ∼130% while the incremental factor of e-CAT is <20%.
e-GST and e-CAT activities in sclerodermic patients grouped in three levels of severity. e-GST activity (U/gHb) and e-CAT (U/mgHb) activity values for healthy subjects taken as control group and for SSc patients divided for DSS (a) and DAI (b). e-GST activity (U/gHb) and e-CAT (U/mgHb) activity values for lcSSc and dcSSc patients divided for DSS (c) and DAI (d). (e) Incremental factor (%) of enzymatic activities for severe stage respect to the control group taken as 0%. Bars represent mean±S.E.M.
e-GST does not correlate to the impairment of a specific organ
Among all organs often damaged by SSc (skin, lung, hearth, kidney, etc.), two are the candidates for a possible correlation with the e-GST expression: kidney and lung. As found in our previous studies, renal failure causes an hyper-expression of e-GST due to the increase of circulating toxins.7, 8 Similarly, hypoxia due to lung damage by SSc may cause accumulation of toxic metabolites, e.g., lactate12 that are normally removed by circulation. Surprisingly, the degree of damage of these specific organs does not correlate with the hyper-expression of e-GST.
Actually, CKD-EPI and eGFR renal parameters do not correlate with e-GST (R2=0.0001, P=0.95 and R2=0.0004, P=0.90, respectively). In addition, intrarenal hemodynamics parameters do not show significant correlations (Pulsatility Index, R2=0.012, P=0.40; Resistive Index, R2=0.014, P=0.35; systolic/diastolic ratio, R2=0.019, P=0.29). By plotting the e-GST found in sclerodermic patients grouped in subgroups based on stages of renal failure according to the Kidney Disease Outcomes Quality Initiative (K/DOQI) guidelines,13 it appears that also at the lowest level of chronic kidney disease (CKD stage 0–I), e-GST is very high and not remarkably different from that found in the CKD stages II and III (Table 3). A comparison of published data obtained with non-sclerodermic nephropathic patients7 confirms this different behavior (Figure 3) that will be discussed extensively below. Paradoxically, patients with limited SSc display a more evident kidney impairment than those with extended disease but a lower value of e-GST activity (Table 1).
e-GST activity for sclerodermic patients grouped in CKD stages. e-GST activity (U/gHb) for healthy subjects and SSc patients (subdivided in CKD renal stages I–III) has been compared with recently published values of e-GST activity (U/gHb) of non-sclerodermic nephropathic patients.7 Bars represent mean±S.E.M.
Other clinical parameters that quantify the impairment of lung do not correlate with e-GST, i.e., ulcers (not shown) and spirometry parameters: diffusion capacity for carbon monoxide (DLCO) (R2=0.0004, P=0.83), forced vital capacity (FVC) (R2=0.033, P=0.068), forced expiratory volume in the first second (FEV1) (R2=0.006, P=0.43), total lung capacity (TLC) (R2=0.032, P=0.072). No correlations of e-GST with lcSSc and dcSSc patients with lung disease (FVC and DLCO<80%) and no lung disease (FVC and DLCO>80%) have been evaluated: e-GST versus lcSSc FVC<80% (R2=0.006, P=0.81); e-GST versus dcSSc FVC<80% (R2=0.013, P=0.68); e-GST versus lcSSc DLCO<80% (R2=0.047, P=0.22); e-GST versus dcSSc DLCO<80% (R2=0.07, P=0.18); e-GST versus lcSSc FVC>80% (R2=0.07, P=0.07); e-GST versus dcSSc FVC>80% (R2=0.005, P=0.72); e-GST versus lcSSc DLCO>80% (R2=0.036, P=0.38); e-GST versus dcSSc DLCO>80% (R2=0.0006, P=0.93).
The influence of systolic pulmonary arterial pressure (sPAP) on e-GST expression has been assessed finding no correlation: e-GST versus lcSSc sPAP<45 mm Hg (R2=0.003, P=0.69); e-GST versus dcSSc sPAP<45 mm Hg (R2=0.034, P=0.24). SSc patients with hypertension (sPAP>45 mm Hg) are the 6% of the total and so no correlation was applied.
Another clinical parameter that quantifies the severity of SSc is the modified Rodnan Skin Score (mRSS) that displays a moderate significant correlation with e-GST (R2=0.14, P<0.0001) for all SSc patients. The correlation of e-GST versus dcSSc mRSS (R2=0.29, P=0.0002) slightly increases when compared with that found for lcSSc mRSS (R2=0.0005, P=0.87).
Finally, no correlation was also found between the disease duration of dcSSc patients and e-GST activity: e-GST versus dcSSc disease duration (years) (R2=0.04, P=0.18); e-GST versus dcSSc disease duration (≤4 years) (R2=0.07, P=0.56); e-GST versus dcSSc disease duration (>4 years) (R2=0.05, P=0.18).
Spearman’s correlation analysis performed for all data sets reveals only slight differences for e-GST versus total SSc DSS (rS=0.72, P<0.0001), e-GST versus total SSc DAI (rS=0.76, P<0.0001), e-GST versus dcSSc DSS (rS=0.79, P<0.0001) and e-GST versus dcSSc DAI (rS=0.75, P<0.0001).
Discussion
In this study, a biochemical parameter, that is, e-GST, has been found to correlate significantly with both severity and activity of SSc (Figure 1). This finding is of particular relevance because DSS and DAI indices are the sum of parameters, which quantify many reversible and irreversible damages or malfunctions of different organs. The SSc organ involvement, evaluated separately, does not correlate with the e-GST expression both for all SSc patients and for lcSSc and dcSSc subgroups except for e-GST versus dcSSc mRSS (R2=0.29, P=0.0002).
Actually, e-GST is a biomarker of blood toxins and a possible biosensor of the nephropathic diseases. In our study, we did not observe a correlation between e-GST and renal damage. We obtained different indications, observing an increased level of e-GST even when the renal function is not impaired (CKD stage 0–I; Figure 3). In this stage, a similar or even higher concentration of e-GST is found compared with that recovered in stage II and III (Figure 3 and Table 3). This almost paradoxical result has been confirmed by observing that patients affected by limited SSc display a lower eGFR and lower e-GST expression compared with that found in the diffuse disease (Table 1). These data deeply differ from those described in non-sclerodermic patients affected by renal diseases (Figure 3) and could be tentatively explained by assuming that e-GST hyper-expression reveals a very early renal damage not revealed by the K/DOQI stage. Alternatively, e-GST hyper-expression could be due to an unknown factor that triggers impairments of specific organs but it is not caused by them. For example, the presence or progressive accumulation of single or selected toxins could trigger this autoimmune disease and also stimulate the hyper-expression of e-GST, simulating what occurs in non-sclerodermic nephropathic patients7, 8 or in subjects living in polluted environments.6 The target organ that will be damaged by the autoimmune disease (kidney and/or lung and/or heart, etc) could be determined on the basis of genetic predisposition or only by random factors. In this case, e-GST hyper-expression in SSc seems to suggest the presence of toxins as the possible cause of this disease, as proposed previously.4, 14, 15
The alternative possibility that e-GST hyper-expression in SSc may be linked to oxidative stress is unlikely. A higher intracellular production of ROS by fibroblasts in sclerodermic patients has actually been observed, and it derives from the activation of an NADPH oxidase-like system. It appears essential to fibroblast proliferation and expression of type I collagen genes in SSc cells.16 However, erythrocytes of SSc patients do not seem to be sensitive to the ROS production occurring in the skin cells or in other tissues. In fact, the activity of catalase, a well-known biomarker of intracellular oxidative stress, displays similar values in healthy subjects as well as in limited and diffuse SSc patients (Table 1 and Figure 2). Furthermore, a different marker for oxidative stress, the Endothelial Dysfunction Index evaluated by FMD, is not correlated to e-GST.
Apart from the stimulating suggestions about the origin of SSc coming from the e-GST hyper-expression, this enzyme may be also proposed as a new biomarker to assess the severity of this disease. By considering that the assay procedure is noninvasive (it requires only a drop a blood), simple, rapid and economic (it needs only a spectrophotometer and the analysis can be done within 2 min), e-GST can be used routinely as a complementary test for monitoring the progress of the disease or to check the efficiency of new therapeutic strategies.
Materials and Methods
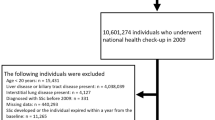
Subjects
A total of 102 patients (90 female and 12 male; mean age 55.5 years, duration of Raynaud’s phenomenon 10.3 years, duration of SSc 9.0 years) fulfilling the American College of Rheumatology criteria for the classification of SSc11 were enrolled in this study. Of them, 58 patients had limited cutaneous SSc and 44 had diffuse cutaneous SSc as defined in literature.1 Patients with a history of uncontrolled systemic hypertension, hyperlipidaemia, cardiac failure, hepatic failure, kidney diseases, diabetes, cerebrovascular diseases, peripheral vascular diseases, or coagulopathy, as well as smokers and pregnant or breastfeeding women, were excluded.
All SSc patients underwent treatment with calcium channel blockers (nifedipine 30 mg/day) for treatment of Raynaud’s phenomenon. Patients in treatment with calcium channel blockers and ACE inhibitors were excluded. Therapy with calcium channel blockers was discontinued 72 h before the renal Doppler ultrasound. None of the patients were in treatment with immunosuppressive drugs (e.g., cyclophosphamide, mycophenolate mofetil) except for 10 mg of prednisone.
A total of 300 healthy subjects (120 female and 180 male, mean age 45 years) were also recruited. The subjects’ written consent was obtained according to the Declaration of Helsinki and the study was approved by the Ethics committee of Sapienza University.
Clinical assessment
Patients underwent clinical assessment and the organs involved in SSc were exhaustively investigated in each patient. Currently, mRSS is the most used method to asses skin induration in SSc. It is determined at a standardized location of 17 different sites of the body with a standardized pinching method and it is scored from 0 to 3.17 Disease activity in SSc was measured using Valentini’s Scleroderma Disease Activity Index (DAI), which consists of 10 weighted variables: total skin score >14, scleroderma, digital necrosis, arthritis, total lung capacity <80%, erythrocyte sedimentation rate>30, hypocomplementemia and change in cardiopulmonary, skin and vascular symptoms in the past month.18 Disease severity was measured using Medsger Scleroderma Disease Severity Scale (DSS). The original scale assessed disease severity in nine organs or systems, namely general health, peripheral vascular, skin, joint/tendon, muscle and gastrointestinal tract, lungs, heart and kidneys. Each organ/system is scored separately from 0 to 4 depending on whether there is no, mild, moderate, severe or end-stage involvement.19 Our patients were divided on the basis of vascular domain: history of Raynaud’s scored 1 (mild), digital pitting scars scored 2 (moderate), digital ulcerations scored 3 (severe) and digital gangrene scored 4 (end-stage).19 Pulmonary function was tested by FVC, TLC, FEV1 and DLCO. The presence/absence of interstitial lung disease was defined according to the results of pulmonary function tests. DLCO, FVC, FEV1 and TLC, expressed as percentages of the predicted normal values, were measured according to the European Respiratory Society guidelines. A value of FVC and DLCO below 80% of the predicted was considered index of restrictive lung disease.20
Echocardiography was performed by a senior cardiologist according to the European Society of Cardiology recommendations. sPAP was measured based on the tricuspid and/or pulmonary regurgitation, adding 10 mm Hg for auricular pressure. Pulmonary hypertension was defined as sPAP >45 mm Hg on cardiac echocardiography and confirmed with right cardiac catheterization pressure measurement (>25 mm Hg).21
Nailfold videocapillaroscopy
Nailfold videocapillaroscopy was performed with a videocapillaroscope (Pinnacle Studio Version 8) equipped with a × 500 optical probe. The nailfold of the second, third, fourth and fifth finger was examined in each patient. According to a previous study,22 the patterns identified within the ‘SSc pattern’ include: early, active and late.
Laboratory parameters
Standard laboratory measurements included serum creatinine, blood urea nitrogen and erythrocyte sedimentation rate. Furthermore, glomerular filtration rate (GFR) was estimated using the CKD-EPI equation.23 Stages of renal failure were diagnosed according to the K/DOQI guidelines.13
Flow-mediated dilation
Endothelial function was assessed using FMD.24 The patients should fast for at least 8–12 h before the study, and they should be studied in a quiet, temperature-controlled room. The subjects were instructed to abstain from eating, smoking, vitamin C and caffeine consumption for at least 4–6 h before the start of the study, and to lie down for 20 min. FMD measurement on the brachial artery was evaluated by ultrasound Toshiba Aplio Ultrasound System SSA-790 (Tokio, Japan) with linear probe from 7.5–10 MHz. Timing of each image frame with respect to the cardiac cycle is determined by simultaneous electrocardiography recording on the ultrasound system video monitor. The subject is positioned supine with the arm in a comfortable position for imaging the brachial artery (antecubital fossa). After baseline diameter measurements for 30 s, the cuff is inflated to 50 mm Hg above the patient’s systolic blood pressure for 5 min, and then deflated. The diameter of the brachial artery was continuously recorded for 2 min after the cuff was deflated. All diameters were measured in the end-diastolic phase, which was defined as the beginning of the R wave on electrocardiography. FMD is typically expressed as the change in post-stimulus diameter as a percentage of the baseline diameter. FMD=[(diameter post-hyperemia−basal diameter)/ basal diameter] × 100. They are considered normal values of FMD if greater than 10%.24
Doppler ultrasound
SSc patients and healthy controls were asked to lie down for at least 15 min before the Doppler ultrasound examination. Renal Doppler ultrasound was performed using a Toshiba Aplio Ultrasound System SSA-790 (Tokyo, Japan) equipped with convex 3.5-MHz probe. Renal Doppler flow was obtained from the interlobar arteries by placing the probe at three different positions (mesorenal, superior and inferior pole) over both kidneys, guided by color flow mapping. Doppler ultrasound examinations were performed by a single investigator, blinded to the clinical features of the patient. The sweep time was set to the highest possible value (100 mm/s) with the lowest spectral filter. The gain was set such that background echoes were barely visible. The Doppler gate width was kept small, and the angle of insonation was maintained at or lower than 60°. We used an anterior approach for detecting the renal artery origin and an oblique, lateral approach for the intermediate tract and intrarenal vessels. The following parameters were measured: Resistive Index, Pulsatility Index and systolic/diastolic ratio.25 Resistive Index was calculated as (peak systolic frequency shift−minimum diastolic frequency shift)/peak systolic frequency shift; Pulsatility Index was calculated as (peak systolic frequency shift−minimum diastolic frequency shift)/mean frequency shift. The average of three measurements for each Doppler parameter of interlobar arteries in both kidneys was calculated.25
Blood samples
Blood samples were collected from the anticubital vein both in healthy subjects and in sclerodermic patients. For enzymatic activity determinations, samples were stored into K-3-EDTA tubes at 4 °C for no more than 2 days.
Enzymatic activities
e-GST activity in total blood was determined with a spectrophotometric assay essentially as described previously.7 Briefly, one volume (40 μl) of whole blood was diluted in 25 volumes (1 ml) of bi-distilled water. After 2 min, 0.1 ml of hemolyzed samples were incubated with 1 mM glutathione and 1 mM of 1-chloro-2,4-dinitrobenzene in 1 ml of 0.1 M potassium-phosphate buffer, pH 6.5. The enzymatic activity was followed (37 °C) at 340 nm where the enzymatic product, the S-glutathionyl-2,4-dinitrobenzene, absorbs (ɛ340 nm=9600 M/cm). For each spectrophotometric determination, the spontaneous reaction of glutathione with 1-chloro-2,4-dinitrobenzene was subtracted. e-GST activity was expressed as enzymatic units (U) at 37 °C and normalized per grams of hemoglobin (Hb) determined in the same blood sample, as reported in literature.7 For catalase determinations, blood samples were collected as described above. Enzyme activity was measured spectrophotometrically at 240 nm (25 °C), evaluating the disappearance of hydrogen peroxide. The extinction coefficient for hydrogen peroxide at 240 nm is 43.6 M/cm. The assay test contained 5 μl of hemolyzed blood sample, 10 mM H2O2 in 0.05 M potassium-phosphate buffer, pH 7.0 containing EDTA 10−4 M. e-CAT activity was expressed as enzymatic units (U) at 25 °C and normalized per milligram of Hb determined in the same blood sample as reported in literature.7 The procedure was also performed using an automated apparatus as described previously.7 Importantly, the activity of e-GST is linearly related to its expression.7, 26 Thus, the increase of e-GSTs activity can be considered equivalent to the hyper-expression of e-GST.
Statistical analysis
After analytical procedures, all patients data have been analyzed. Data are expressed as mean±S.E.M. Unpaired t-test was employed to compare data between various groups; nonparameter variables were analyzed by Mann–Whitney test. A value of P<0.05 was considered statistically significant. Spearman’s rank correlation coefficient (rS) analysis has been performed on all data sets. Data were processed using statistical software MedCalc (Mariakerke, Belgium). Passing–Bablock regression analysis was performed according to the original protocol.27
Abbreviations
- DAI:
-
Valentini’s Scleroderma Disease Activity Index
- dcSSc:
-
diffuse cutaneous SSc
- DLCO:
-
diffusion capacity for carbon monoxide
- DSS:
-
Medsger scleroderma disease severity scale
- e-CAT:
-
erythrocyte catalase
- eGFR:
-
estimated glomerular filtration rate
- e-GST:
-
erythrocyte glutathione transferase
- FEV1:
-
forced expiratory volume in the first second
- FMD:
-
flow-mediated dilation
- FVC:
-
Forced vital capacity
- Hb:
-
hemoglobin
- lcSSc:
-
limited cutaneous SSc
- mRSS:
-
modified Rodnan skin score
- SSc:
-
systemic sclerosis
- TLC:
-
total lung capacity
References
LeRoy EC, Black C, Fleischmajer R, Jablonska S, Krieg T, Medsger TA Jr et al. Scleroderma (systemic sclerosis): classification, subsets and pathogenesis. J Rheumatol 1988; 15: 202–205.
Gabrielli A, Avvedimento EV, Krieg T . Scleroderma. N Engl J Med 2009; 360: 1989–2003.
Klippel JH, Stone JH, Crofford LJ, White PH . Primer on the Rheumatic Diseases 13th edn Springer Science, Arthritis Foundation: Atlanta, GA, 2008.
Broen JC, Coenen MJ, Radstake TR . Genetics of systemic sclerosis: an update. Curr Rheumatol Rep 2012; 14: 11–21.
Hayes JD, Flanagan JU, Jowsey RI . Glutathione transferases. Annu Rev Pharmacol Toxicol 2005; 45: 51–88.
Fabrini R, Bocedi A, Del Grosso E, Morici L, Federici G, Palleschi A et al. Erythrocyte glutathione transferase: a novel biomarker to check environmental pollution hazardous for humans. Biochem Biophys Res Commun 2012; 426: 71–75.
Dessì M, Noce A, Dawood KF, Galli F, Taccone-Gallucci M, Fabrini R et al. Erythrocyte glutathione transferase: a potential new biomarker in chronic kidney diseases which correlates with plasma homocysteine. Amino Acids 2012; 43: 347–354.
Noce A, Ferrannini M, Fabrini R, Bocedi A, Dessì M, Galli F et al. Erythrocyte glutathione transferase: a new biomarker for hemodialysis adequacy, overcoming the Kt/V(urea) dogma? Cell Death Dis 2012; 23: e377.
Steen VD . Scleroderma renal crisis. Rheum Dis Clin North Am 2003; 29: 315–333.
Steen VD, Medsger TA . Changes in causes of death in systemic sclerosis, 1972-2002. Ann Rheum Dis 2007; 66: 940–944.
Masi AT and Subcommittee for Scleroderma criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee. Preliminary criteria for the classification of Systemic Sclerosis (Scleroderma). Arthritis Rheum 1980; 23: 581–590.
James JH, Luchette FA, McCarter FD, Fischer JE . Lactate is an unreliable indicator of tissue hypoxia in injury or sepsis. Lancet 1999; 354: 505–508.
National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002; 39: S1–S266.
Farhat SC, Silva CA, Orione MA, Campos LM, Sallum AM, Braga AL . Air pollution in autoimmune rheumatic diseases: a review. Autoimmun Rev 2011; 11: 14–21.
Jimenez SA, Derk CT . Following the molecular pathways toward an understanding of the pathogenesis of systemic sclerosis. Ann Intern Med 2004; 140: 37–50.
Sambo P, Baroni SS, Luchetti M, Paroncini P, Dusi S, Orlandini G et al. Oxidative stress in scleroderma: maintenance of scleroderma fibroblast phenotype by the constitutive up-regulation of reactive oxygen species generation through the NADPH oxidase complex pathway. Arthritis Rheum 2001; 44: 2653–2664.
Clements P, Lachenbruch P, Siebold J, White B, Weiner S, Martin R et al. Inter and intraobserver variability of the total thickness score (modified Rodnan TSS) in systemic sclerosis. J Rheumatol 1995; 22: 1281–1285.
Medsger TA Jr, Bombardieri S, Czirjak L, Scorza R, Della Rossa A, Bencivelli W . Assessment of severity and prognosis. Clin Exp Rheumatol 2003; 21 (Suppl 29): 42–46.
Valentini G, Silman AJ, Veale D . Assessment of disease activity. Clin Exp Rheumatol 2003; 21 (Suppl 29): 39–41.
Roca J, Whipp B . ERS Task Force on Standardization of Clinical Exercise Testing. Clinical exercise testing with reference to lung disease: indications, standardization and interpretation strategies. Eur Respir J 1997; 10: 2662–2689.
Galiè N, Torbicki A, Barst R, Dartevelle P, Haworth S, Higenbottam T et al. Guidelines on diagnosis and treatment of pulmonary arterial hypertension. The Task Force on Diagnosis and Treatment of Pulmonary Arterial Hypertension of the European Society of Cardiology. Eur Heart J 2004; 25: 2243–2278.
Cutolo M, Sulli A, Secchi ME, Paolino S, Pizzorni C . Nailfold capillaroscopy is useful for the diagnosis and follow-up of autoimmune rheumatic diseases. A future tool for the analysis of microvascular heart involvement? Rheumatology 2006; 45 (Suppl 4): 43–46.
Gigante A, Rosato E, Massa R, Rossi C, Barbano B, Cianci R et al. Evaluation of Chronic Kidney Disease Epidemiology Collaboration equation to estimate glomerular filtration rate in scleroderma patients. Rheumatology (Oxford) 2012; 51: 1426–1431.
Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: A report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol 2002; 39: 257–265.
Rosato E, Gigante A, Barbano B, Cianci R, Molinaro I, Rossi C et al. Intrarenal hemodynamic parameters correlate with glomerular filtration rate and digital microvascular damage in patients with systemic sclerosis. Semin Arthritis Rheum 2012; 41: 815–821.
Galli F, Rovidati S, Benedetti S, Buoncristiani U, Covarelli C, Floridi A et al. Overexpression of erythrocyte glutathione-S-transferase in uremia and dialysis. Clin Chem 1999; 45: 1781–1788.
Passing H, Bablock W . Comparison of several regression procedures for method comparison studies and determination of sample size. Application of linear regression procedures for method comparison studies in clinical chemistry, Part II. J Clin Chem Clin Biochem 1984; 22: 431–445.
Acknowledgements
We thank ‘Fondazione Roma—Terzo settore’ for funding the present research. We also thank Professor Jens Pedersen for critical reading of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by A Stephanou
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Fabrini, R., Rosato, E., Gigante, A. et al. Erythrocyte glutathione transferase: a non-antibody biomarker for systemic sclerosis, which correlates with severity and activity of the disease. Cell Death Dis 4, e736 (2013). https://doi.org/10.1038/cddis.2013.255
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cddis.2013.255
Keywords
This article is cited by
-
Erythrocyte glutathione transferase in kidney transplantation: a probe for kidney detoxification efficiency
Cell Death & Disease (2018)