Abstract
Objective: Pain intensity and the plasma concentrations of metoprolol and its major metabolite α-hydroxymetoprolol as well as noradrenaline (NA), adrenaline (A) and neuropeptide Y (NPY) were determined in patients with pain due to definite or suspected acute myocardial infarction (AMI) after graded metoprolol infusion. Pain intensity and metoprolol kinetics were assessed over 8 h.
Methods: Twenty-seven patients of either sex, aged 48–84 years with ongoing chest pain upon arrival to the Coronary Care Unit (CCU) were subdivided into two groups: (1) patients with ECG signs of threatening transmural myocardial damage (n=15); and (2) patients without such ECG signs (n=12). Pain intensity was assessed by a numerical rating scale (NRS) and venous blood was obtained for determination of plasma catecholamine and NPY concentrations. A continuous infusion of metoprolol (3 mg · min−1 i.v) was started and serial blood samples for plasma catecholamines, NPY as well as metoprolol and its major metabolite α-hydroxymetoprolol were obtained from the contralateral arm.
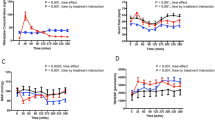
Results: Initial pain intensity was 5.9 (arbitrary units) and 5.4 in the groups with and without signs of transmural myocardial damage, respectively. One third of the patients with ST changes reported full pain relief (NRS=0) within 70 min after starting metoprolol infusion (accumulated dose, 15–180 mg). Among the patients without ST changes upon arrival, full pain relief was obtained in 70% (accumulated dose, 30–120 mg). There was a dose-dependent relation between accumulated metoprolol dose and pain relief. The diagnosis of acute myocardial infarction (AMI) was confirmed in all 15 patients with ECG signs on arrival of transmural myocardial damage. The mean metoprolol dose in this group was 91(12) mg. The mean metoprolol dose in the 12 patients without ST changes was 64(8) mg. In all, seven of these patients developed definite AMI.
The terminal half-life of unchanged metoprolol ranged from 2.5 to 8.5 h in group 1 and from 2.2 to 5.2 h in group 2. In group 1, metoprolol half-life was 4.5 h and total plasma clearance (CL) 54.1 l · h−1. In group 2, the metoprolol half-life was 3.7 h and total plasma clearance 75.4 l · h−1. There was a significant difference in clearance between the groups.
After the intravenous metoprolol infusion, α-hydroxymetoprolol concentrations increased gradually. In groups 1 and 2, maximal concentrations in plasma (Cmax) were 143 and 135 nmol · l−1 for α-hydroxymetoprolol and 2830 and 1653 nmol · l−1 for metoprolol, respectively.
Plasma NA or NPY did not differ between the groups. In contrast, plasma A was significantly higher during the initial 90 min of observation in patients with ECG signs of transmural myocardial damage.
Conclusion: High-dose intravenous metoprolol was well tolerated in patients with suspected AMI. There was a more rapid and almost complete pain relief in patients without signs of transmural ischaemia compared with the patients with ECG signs of transmural AMI at arrival. In the later group of patients, plasma clearance of metoprolol was significantly reduced.
Similar content being viewed by others
Author information
Authors and Affiliations
Additional information
Received: 23 August 1996 / Accepted in revised form: 6 March 1997
Rights and permissions
About this article
Cite this article
Everts, B., Karlson, B., Herlitz, J. et al. Effects and pharmacokinetics of high dose metoprolol on chest pain in patients with suspected or definite acute myocardial infarction. E J Clin Pharmacol 53, 23–31 (1997). https://doi.org/10.1007/s002280050332
Issue Date:
DOI: https://doi.org/10.1007/s002280050332