Summary
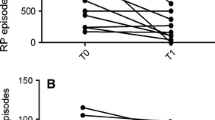
Ten patients with moderate to severe Raynaud’s syndrome were recruited into a four week randomised double blind crossover study to compare the efficacy of UK-38,485 50 mg, a new thromboxane synthetase inhibitor with that of placebo. With the doses used there was no significant difference between the two treatment periods in the number, severity and duration of ischaemic attacks, the mean hand temperatures, forearm and digital blood flow and red blood cell rheology.
Similar content being viewed by others
References
Dowd PM, Martin MFR, Cooke ED, Bowcock SA, Dieppe PA, Kirby JDT (1982) Treatment of Raynaud’s phenomenon by intravenous infusion of prostacyclin (PGI2). Br J Dermatol 106: 81–89
Belch JJF, Drury JK, Capell H, Forbes CD, Newman P, McKenzie F, Lieberman P, Prentice CRM (1983) Intermittent epoprostenol (prostacyclin) infusion in patients with Raynaud’s syndrome. Lancet 1: 313–315
Kahaleh MB, Osborn I, LeRoy EC (1982) Elevated levels of circulating platelet aggregates and beta-thromboglobulin in scleroderma. Ann Int Med 96: 610–613
Parry MJ, Randall MJ, Hawkeswood E, Cross PE, Dickinson RP (1982) Enhanced production of prostacyclin in blood after treatment with selective thromboxane synthetase inhibitor, UK-38,485. Br J Pharmacol 77: 547P
Fischer S, Struppler M, Bohlig B, Bernutz C, Wober W, Weber PC (1983) The influence of selective thromboxane synthetase inhibition with a novel imidazole derivative, UK-38,485, on prostanoid formation in man. Circulation 68: 821–826
Orchard MA, Blair IA, Dollery CT, Lewis PJ (1983) Blood can synthesise prostacyclin. Lancet 2: 565
Belch JJF, Cormie J, Newman P, McLaren M, Barbenell J, Capell H, Lieberman P, Forbes CD, Prentice CRM (1983) Dazoxiben, a thromboxane synthetase inhibitor in the treatment of Raynaud’s syndrome: a double-blind trial. Br J Clin Pharmacol 15: 113s-116s
Subcommittee for Scleroderma Criteria of the American Rheumatism Association Diagnostic and Therapeutic Criteria Committee (1980) Preliminary criteria for the classification of systemic sclerosis. Arthritis Rheum 23: 581–590
Cooke ED, Bowcock SA, Smith AT (1984) A mathematical model for the vascular behaviour of the hands in response to cold stress. Vascular diagnosis and therapy (in press)
Challoner AVJ, Ramsay CA (1974) A photoelectric plethysmograph for the measurement of cutaneous blood flow. Phys Med Biol 19: 317–328
Kovacs IB, Sowemimo-Coker SO, Kirby JDT, Turner P (1983) Altered behaviour of erythrocytes in scleroderma. Clin Sci 65: 515–519
Streichman S, Segal E, Tatarsky I, Marmur A (1981) Moving boundary electrophoresis and sialic acid content of normal and polycythaemic red blood cells. Br J Haematol 48: 273–279
Bertele V, Cerletti C, Schieppatia A, Di Minno G, De Gaetano G (1981) Inhibition of thromboxane synthetase does not necessarily prevent platelet aggregation. Lancet 1: 1057–1058
Bertele V, Tomasiak M, Falanga A, Cerletti C, De Gaetano G (1982) Aspirin inhibits platelet aggregation but not because it prevents thromboxane synthesis. Lancet 2: 775
Nijkamp FP, Moncada S, White HL, Vane JR (1977) Diversion of prostaglandin endoperoxide metabolism by selective inhibition of Thromboxane A2 biosynthesis in lung, spleen or platelets. Eur J Pharmacol 44: 179–186
Needleman P, Wyche A, Raz A (1979) Platelet and blood vessel arachidonate metabolism and interactions. J Clin Invest 63: 345–349
Fitzgerald GA, Brash AR, Oates JA (1983) Endogenous prostacyclin biosynthesis and platelet function during selective inhibition of thromboxane synthase in man. J Clin Invest 71: 1336–1343
Tyler HM, Saxton CAPD, Parry MJ (1981) Administration to man of UK-37,248-01, a selective inhibitor of thromboxane synthetase. Lancet 1: 629–632
Miller OV, Gorman RR (1979) Evidence for distinct prostaglandin I2 and D2 receptors in human platelets. J Pharmacol Exp Ther 210: 134–140
Vermylen J, Deckmyn H (1983) Reorientation of prostaglandin endoperoxide metabolism by a thromboxane synthetase inhibitor: in vitro and clinical observations. Br J Clin Pharmacol 15: 17s-22s.
Dowd PM, Kovacs IB, Bland CJH, Kirby JDT (1981) Effect of prostaglandins I2 and E1 on red cell deformability in patients with Raynaud’s phenomenon and systemic sclerosis. Br Med J 283: 350
Kovacs IB, O’Grady J (1984) Prostacyclin increases filterability of normal and rigidified human red blood cells in vitro. Agents Actions 14: 306–310
Horrobin DF, Jenkins K, Manku MS (1983) Raynaud’s phenomenon, histamine, and prostaglandins. Lancet 1: 747–748
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Rustin, M.H.A., Grimes, S.M., Kovacs, I.B. et al. A double blind trial of UK-38,485, an orally active thromboxane synthetase inhibitor, in the treatment of Raynaud’s syndrome. Eur J Clin Pharmacol 27, 61–65 (1984). https://doi.org/10.1007/BF02395208
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF02395208