Abstract
Objectives
To investigate the indications of high-flow nasal cannula (HFNC) oxygen therapy among patients with mild hypercapnia and to explore the predictors of intubation when HFNC fails.
Methods
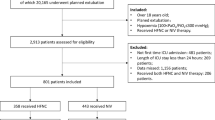
This retrospective study was conducted based on the Medical Information Mart for Intensive Care IV (MIMIC-IV) database. Adult patients with mild hypercapnia (45 < PaCO2 ≤ 60 mmHg) received either HFNC or non-invasive ventilation (NIV) oxygen therapy. Propensity score matching (PSM) was implemented to increase between-group comparability. The Kaplan–Meier method was used to estimate overall survival and cumulative intubation rates, while 28-day mortality and 48-h and 28-day intubation rates were compared using the Chi-squared test. The predictive performances of HR/SpO2 and the ROX index (the ratio of SpO2/FiO2 to respiratory rate) at 4 h were assessed regarding HFNC failure, which was determined if intubation was given within 48 h after the initiation of oxygen therapy. The area under the receiver operating characteristic curve (AUC) for HR/SpO2 and the ROX index were calculated and compared.
Results
A total of 524,520 inpatient hospitalization records were screened, 106 patients in HFNC group and 106 patients in NIV group were successfully matched. No significant difference in 48-h intubation rate between the HFNC group (the treatment group) and the NIV group (the control group) (14.2% vs. 8.5%, p = 0.278); patients receiving HFNC had higher 28-day intubation rate (26.4% vs. 14.2%, p = 0.029), higher 28-day mortality (17.9% vs. 8.5%, p = 0.043), and longer ICU length of stay (4.4 vs. 3.3 days, p = 0.019), compared to those of NIV group. The AUC of HR/SpO2 at 4 h after the initiation of HFNC yielded around 0.660 for predicting 48-h intubation, greater than that of the ROX index with an AUC of 0.589 (p < 0.01).
Conclusion
Patients with impending respiratory failure had lower intubation rate, shorter ICU length of stay, and lower mortality when treated mild hypercapnia with NIV over HFNC. As opposed to the ROX index, a modest, yet improved predictive performance is demonstrated using HR/SpO2 in predicting the failure of HFNC among these patients.
Similar content being viewed by others
Introduction
High-flow nasal cannula (HFNC) oxygen therapy has been widely applied, delivering a heated and humidified high-flow air-oxygen mixture, which has been shown to outperform conventional oxygen therapy [1,2,3]. Several clinical trials have suggested that the effect of HFNC in patients with hypoxemia is not inferior to that of non-invasive ventilation (NIV) [4,5,6]. However, only a few studies have reported that HFNC can achieve the same therapeutic effect as NIV among patients with mild hypercapnia [7, 8]. Whether HFNC can replace NIV in treating mild hypercapnia is still unclear, while predictors at an early stage for the outcome of oxygen therapy remain to be explored.
This study retrospectively analyzed patients derived from the Medical Information Mart for Intensive Care IV (MIMIC-IV) database to investigate the indications of HFNC for patients with mild hypercapnia. The predictive performance of physiological parameters for the outcome of high-flow therapy was also evaluated.
Methods
Patients
Patients admitted to ICU from 2008 to 2019 were identified in the MIMIC-IV database. The inclusion criteria were as follows: over 18 years old; with mild hypercapnia (45 < PaCO2 ≤ 60 mmHg) before HFNC or NIV. The exclusion criteria were as follows: tracheotomy; without intubation plan; having received both HFNC and NIV before intubation.
Source of Data and Ethics Approval
This retrospective study was conducted based on the MIMIC-IV database [9], consisting of comprehensive and high-quality data of patients admitted to the intensive care unit (ICU) at the Beth Israel Deaconess Medical Center between 2008 and 2019 with pre-existing institutional review board approval. One author (QZ) obtained access to the database and was responsible for data extraction.
Study Design
Patients were treated with either HFNC or NIV (continuously or intermittently). The following data were extracted from the database: age, sex, body mass index (BMI), diagnosis and chronic comorbidities, Charlson Comorbidity Index, Simplified Acute Physiology Score II (SAPS-II) at ICU admission, physiological parameters at baseline and within 24 h after the initiation of oxygen therapy, as well as outcome measures including 28-day mortality, 48-h and 28-day intubation rates, and length of stay in ICU and in hospital. Patients were matched using a propensity score model. Treatment outcomes regarding mortality, intubation rates, and length of stay between the HFNC group (the treatment group) and the NIV group (the control group) were compared after propensity score matching (PSM).
HR/SpO2 (the ratio of heart to pulse oxygen saturation) at 4 h was used as a predictor for high-flow treatment failure, defined as receiving intubation within 48 h after the initiation of the treatment. Its predictive performance was compared with the 4-h ROX index (the ratio of SpO2/FiO2 to respiratory rate) using the area under the receiver operating characteristic curve (AUC).
Statistical Analysis
Variables with normal distributions were presented as means (SD) and were compared by independent samples t test. Non-normally distributed variables were reported as medians [IQR], where the Mann–Whitney U test was used. Categorical variables were described as percentages and were compared using the Chi-squared test or Fisher's exact test, when appropriate. The Kaplan–Meier method was applied to estimate the overall survival rate and cumulative intubation rate.
Missing values were imputed by Multivariate Imputation by Chained Equations, following which a multivariate logistic regression model incorporating was constructed to estimate a patient’s propensity score for receiving HFNC. 1:1 nearest neighbor matching with a caliper width of 0.1 was then applied [10].
All statistical analyses were performed with R (version 3.6.1), and a p value less than 0.05 was considered statistically significant.
Results
A total of 524,520 hospitalization records were screened and 379 patients were included in this study, of which 133 patients received HFNC and 246 patients received NIV. After propensity score matching, there were 106 patients in the HFNC group and 106 patients in the NIV group, with a mean age of 68.8 and 66.1 years old, respectively. PaCO2 before oxygen therapy was 49.8 [46.8, 57.5] mmHg in the HFNC group and 48.8 [46.5, 56.5] mmHg in the NIV group. No statistically significant differences were identified in baseline characteristics regarding age, sex, BMI, diagnosis and chronic comorbidities, SAPS II, and Charlson score between the two groups (all p > 0.05).
There was no significant difference in 48-h intubation rate between the HFNC group and the NIV group after PSM (14.2% vs. 8.5%, p = 0.278). However, patients on HFNC appeared to have higher 28-day intubation rate (26.4% vs. 14.2%, p = 0.029), had higher 28-day mortality (17.9% vs. 8.5%, p = 0.043), and stayed longer in ICU (4.4 vs. 3.3 days, p = 0.019) as opposed to those receiving NIV therapy (Table 1 and Fig. 1).
Heart rate and respiratory rate at 12 h in the HFNC group significantly decreased as compared with those at baseline (91.2 vs. 96.0 and 21.7 vs. 22.3, both p < 0.05). PaCO2 at 24 h in the HFNC group significantly decreased compared to that at baseline (45.9 vs. 49.8 mmHg, p < 0.05), while in the NIV group, PaCO2 at 12 h was significantly lower than that at baseline (46.0 vs. 48.8 mmHg, p < 0.05). (Table 2 and Fig. 2).
No significant difference in 48-h intubation rate between the HFNC group (the treatment group) and the NIV group (the control group) (14.2% vs. 8.5%, p = 0.278); patients receiving HFNC had higher 28-day intubation rate (26.4% vs. 14.2%, p = 0.029), higher 28-day mortality (17.9% vs. 8.5%, p = 0.043), and longer ICU length of stay (4.4 vs. 3.3 days, p = 0.019), compared to those of NIV group (Fig. 3).
Regarding the prediction for 48-h intubation among patients in the HFNC group, the AUC of HR/SpO2 at 4 h after HFNC is greater than that of the ROX index (0.660 vs. 0.589, p < 0.01) (Table 3 and Fig. 3). An optimal cut-off point of HR/SpO2 with a value of 1.08 was determined by the Youden index, resulting in a sensitivity of 57.1% and a specificity of 73.6% (Fig. 4).
Continuous variables were compared by independent samples t test or Mann–Whitney U test, while categorical variables were compared using Chi-squared test or Fisher's exact test, when appropriate.
Discussion
High-flow oxygen therapy provides constant airflow and oxygen concentration, which has been found more effective than conventional oxygen therapies such as nasal catheter and mask oxygen [11,12,13]. For patients with mild to moderate hypoxemia, the effect of HFNC is not inferior to that of NIV [5, 6]. Previous physiological studies have illustrated that high-flow airflow can wash the nasopharyngeal dead space and produce a low level of 3–6 cmH2O positive end-expiratory pressure [14,15,16], which is the theoretical basis for HFNC in the treatment of mild hypercapnia. A few studies have suggested that HFNC can replace NIV for patients with hypercapnia [17, 18], while it is generally not applicable to severe type 2 respiratory failure. However, the small sample sizes in these studies have left the specific indications for HFNC in the treatment of hypercapnia unclear.
More than 500,000 patients with MIMIC-IV data were screened and 379 patients with mild hypercapnia receiving either HFNC or NIV were included in our study. Twenty-eight-day intubation rate and 28-day mortality in the HFNC group were higher than those in the NIV group after propensity score matching. Furthermore, the ICU length of stay in the HFNC group was longer than that in the NIV group. The insignificant difference in 48-h intubation rate between the two groups may be a result of the insufficient event cases. Previous studies have shown that the effect of HFNC outperforms conventional oxygen therapy for patients with hypercapnia [19, 20] and home-based HFNC can also improve the quality of life for patients with stable chronic obstructive pulmonary disease [21].
Our retrospective study demonstrates that HFNC can reduce PCO2 and increase PO2 in patients with mild hypercapnia within a short period of treatment (24 h), as effective as non-invasive ventilator. However, during a longer period, from 7 to 28 days, the intubation rate and mortality of the two groups were different and the effect of the HFNC group was inferior to the NIV group. In addition to PO2 and PCO2, there are many other factors which can lead to intubate, such as the occurrence of underlying disease progression (malignancy, chronic kidney disease, etc.), infection, heart failure, and shock. Therefore, the intubation rate may not be completely consistent with the change of PCO2 within a short period of treatment. Due to limited retrospective data, blood gas analysis only recorded changes within 24 h of treatment initiation in both groups in our study. However, the difference in intubation rate between the two groups was at 48 h and 28 days. Thus, it may suggest that a short period (24 h) of improvement in blood gas analysis is insufficient to indicate that the patient’s treatment is effective and that a longer period of close observation is needed.
Nevertheless, our results indicate that HFNC cannot replace non-invasive ventilator for patients with mild hypercapnia, although it could be an alternative for patients with poor tolerance to non-invasive ventilation. Nearly half of the patients with HFNC failure were intubated within 48 h of treatment [5, 6], while increased mortality was found among patients with delayed intubation due to HFNC failure in a retrospective study [22]. In our study, the differences in intubation rates between the two groups were also significantly enlarged with the prolongation of the treatment. It is also suggested that improper high-flow therapy may delay intubation in patients with hypercapnia. Therefore, the effect of HFNC needs to be evaluated early.
In our study, the changes in physiological parameters within the first 24 h after the beginning of oxygen therapy in the two groups were recorded. The heart rate and respiratory rate significantly decreased at 12 h after initiation of HFNC compared with baseline data. Meanwhile, PaCO2 in both the treatment group and the control group decreased during this period. This therapeutic effect is related to the reduction of respiratory activity and oxygen consumption [23, 24], which suggests the use of vital sign changes for the prediction of HFNC failure to avoid delayed intubation.
In recent years, the ROX index has been proposed as a predictor of HFNC failure, consisting of SpO2, FiO2, and respiratory rate [25]. All three parameters are readily available in clinical settings and their dynamic changes are useful in assessing the success of HFNC. Generally, a ROX index greater than 4.88 indicates the efficacy of HFNC, while a ROX index less than 3.85 indicates the risk of HFNC failure [26]. However, the ROX index does not take into account heart rate change, which is a sensitive physiological parameter in the early stage of respiratory failure and its added predictive value for HFNC failure has been demonstrated in combination with the ROX index [27]. Therefore, the prediction accuracy of the ROX index needs further evaluation. Until now, no studies have verified the predictive value of the ROX index in patients with hypercapnia.
In this study, HR/SpO2 was formulated as a predictor incorporating heart rate and pulse oxygen, which is sensitive, non-invasive, and easy to apply. The HR/SpO2 after 4 h treatment was calculated to predict 48-h intubation rate. It was found that the predictive performance of the ROX index for 48-h intubation after the initiation of HFNC yielded an AUC of less than 0.6, while the HR/SpO2 achieved a greater, yet modest AUC of 0.660. An optimal cut-off value of the ROX index based on the Youden index leads to poor sensitivity and moderate specificity.
Previous studies showed that the ROX index is of certain value in predicting the failure of HFNC resulted in intubation. However, the data in our study suggested that neither ROX index nor HR/SpO2 are good predictors of intubation in patients with mild hypercapnia treated with HFNC. This may be related to the poor specificity of physiological parameters such as RR, HR, and SpO2. Therefore, only 2–3 physiological parameters were included in the prediction index, without more physiological information, which was obviously insufficient to predict the HFNC treatment effects on patients.
In conclusion, the prediction accuracy of HFNC based on early changes in a single physiological parameter is inadequate, and algorithmic models combining more clinical and physiological predictors may improve the accuracy of outcome prediction in subsequent studies.
Limitations
Type 2 respiratory failure is not the main indication of HFNC; as a result, the sample size of HFNC group was substantially reduced in this study. The average values of physiological parameters at each period within 24 h were calculated, which might be insufficient to reflect real-time acuity. In addition, the results of our study need to be verified by prospective studies.
Some literatures reported that bicarbonate levels play an important role in the success or failure of non-invasive ventilator treatment. We tried to collect and analyze the bicarbonate level data, but unfortunately, the data about bicarbonate in the database depended on blood gas analysis which was not frequently reviewed, and there was a lack of data in some enrolled patients, so a systematic analysis about bicarbonate levels could not be made. Therefore, in future studies, we will pay extra attention to the effect of carbonate levels on treatment outcomes.
Conclusion
Patients with impending respiratory failure had lower intubation rate, shorter ICU length of stay, and lower mortality when treated mild hypercapnia with NIV over HFNC. As opposed to the ROX index, a modest, yet improved predictive performance is demonstrated using HR/SpO2 in predicting treatment failure among mild hypercapnia patients receiving HFNC.
Data Availability
The MIMIC-IV data were available on the project website at https://mimic-iv.mit.edu/.
Abbreviations
- HFNC:
-
High-flow nasal cannula
- NIV:
-
Non-invasive ventilation
- MIMIC-IV:
-
Medical information mart for intensive care IV
- ICU:
-
Intensive care unit
- BMI:
-
Body mass index
- SAPS-II:
-
Simplified acute physiology score II
- ABG:
-
Arterial blood gas
- IQR:
-
Interquartile range
- PSM:
-
Propensity score matching
- AUC:
-
Area under the receiver operating characteristic curve
- ROX index:
-
Ratio of SpO2/FiO2 to respiratory rate
References
Nishimura M (2015) High-flow nasal cannula oxygen therapy in adults. J Intensive Care 3(1):15
Groves N, Tobin A (2007) High flow nasal oxygen generates positive airway pressure in adult volunteers. Aust Crit Care 20(4):126–131
Chikata Y et al (2017) FIO2 in an adult model simulating high-flow nasal cannula therapy. Respir Care 62(2):193–198
Frat JP et al (2015) High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med 372(23):2185–2196
Hernandez G et al (2016) Effect of postextubation high-flow nasal cannula vs noninvasive ventilation on reintubation and postextubation respiratory failure in high-risk patients a randomized clinical trial supplemental content. JAMA 316:1565
Stéphan F et al (2015) High-flow nasal oxygen vs noninvasive positive airway pressure in hypoxemic patients after cardiothoracic surgery: a randomized clinical trial. JAMA 313(23):2331–2339
Yang P-L, Yu J-Q, Chen H-B (2021) High-flow nasal cannula for acute exacerbation of chronic obstructive pulmonary disease: a systematic review and meta-analysis. Heart Lung 50(2):252–261
Pantazopoulos I et al (2020) Nasal high flow use in copd patients with hypercapnic respiratory failure: treatment algorithm & review of the literature. COPD 17(1):101–111
Johnson A et al (2020) MIMIC-IV (version 0.4). PhysioNet. https://doi.org/10.13026/a3wn-hq05
Leite W (2016) Practical propensity score methods using R. SAGE Publications Inc, Thousand Oaks
Hernández G et al (2016) Effect of postextubation high-flow nasal cannula vs conventional oxygen therapy on reintubation in low-risk patients: a randomized clinical trial. JAMA 315(13):1354–1361
Wang Y et al (2020) High-flow nasal cannula vs conventional oxygen therapy for postcardiothoracic surgery. Respir Care. https://doi.org/10.4187/respcare.07595
Granton D et al (2020) High-flow nasal cannula compared with conventional oxygen therapy or noninvasive ventilation immediately postextubation: a systematic review and meta-analysis. Crit Care Med 48(11):e1129–e1136
Parke R, McGuinness S, Eccleston M (2009) Nasal high-flow therapy delivers low level positive airway pressure. Br J Anaesth 103(6):886–890
Möller W et al (2015) Nasal high flow clears anatomical dead space in upper airway models. J Appl Physiol 118:jap.00934.2014
Van Hove SC et al (2016) An experimental and numerical investigation of CO2 distribution in the upper airways during nasal high flow therapy. Ann Biomed Eng 44(10):3007–3019
Bräunlich J et al (2019) Nasal high-flow versus noninvasive ventilation in patients with chronic hypercapnic COPD. Int J Chron Obstruct Pulmon Dis 14:1411–1421
Tan D et al (2020) High-flow nasal cannula oxygen therapy versus non-invasive ventilation for chronic obstructive pulmonary disease patients after extubation: a multicenter, randomized controlled trial. Crit Care 24(1):489
Kim E et al (2018) Effectiveness of high-flow nasal cannula oxygen therapy for acute respiratory failure with hypercapnia. J Thorac Dis 10:882–888
Lee H et al (2019) Reduction of PaCO2 by high-flow nasal cannula in acute hypercapnic respiratory failure patients receiving conventional oxygen therapy. Acute and Critical Care 34:202–211
Nagata K et al (2017) Domiciliary high-flow nasal cannula oxygen therapy for stable hypercapnic COPD patients: a multicenter, randomized crossover trial. Ann Am Thorac Soc 15:432
Kang BJ et al (2015) Failure of high-flow nasal cannula therapy may delay intubation and increase mortality. Intensive Care Med 41(4):623–632
Roca O et al (2013) Patients with New York Heart Association class III heart failure may benefit with high flow nasal cannula supportive therapy: high flow nasal cannula in heart failure. J Crit Care 28(5):741–746
Sztrymf B et al (2011) Beneficial effects of humidified high flow nasal oxygen in critical care patients: a prospective pilot study. Intensive Care Med 37(11):1780–1786
Roca O et al (2018) An index combining respiratory rate and oxygenation to predict outcome of nasal high flow therapy. Am J Respir Crit Care Med 199:1368
Spinelli E, Roca O, Mauri T (2020) Dynamic assessment of the ROX index during nasal high flow for early identification of non-responders. J Crit Care 58:130–131
Goh K et al (2020) Early prediction of high flow nasal cannula therapy outcomes using a modified ROX index incorporating heart rate. J Intensive Care 8:41
Acknowledgements
None.
Funding
Effect evaluation and prediction of high-flow nasal cannula oxygen with algorithm model (Grant No. ZMX2020-121).
Author information
Authors and Affiliations
Contributions
LS conceived the idea, interpreted the results, and drafted the manuscript. QZ extracted the data, performed the analysis, and helped to revise the manuscript. YX, WL, and AZ helped to interpret the results and drafted the manuscript. TL helped to conceive the idea, interpreted the results, and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The study was an analysis of two third-party anonymized publicly available databases with pre-existing institutional review board (IRB) approval.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Su, L., Zhao, Q., Liu, T. et al. Efficacy of High-Flow Nasal Cannula Oxygen Therapy in Patients with Mild Hypercapnia. Lung 199, 447–456 (2021). https://doi.org/10.1007/s00408-021-00472-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-021-00472-4